Assessment of biomechanical stability of the thoracolumbar junction with a burst fracture of Th12 following surgical stabilization under rotational loading
DOI:
https://doi.org/10.15587/2519-4798.2024.306367Keywords:
Thoracolumbar junction, traumatic injury, transpedicular fixation, burst fracture, rotational loadingAbstract
The thoracolumbar junction is the most vulnerable to traumatic injuries, with over 65 % of injuries to the thoracolumbar spine occurring in this region.
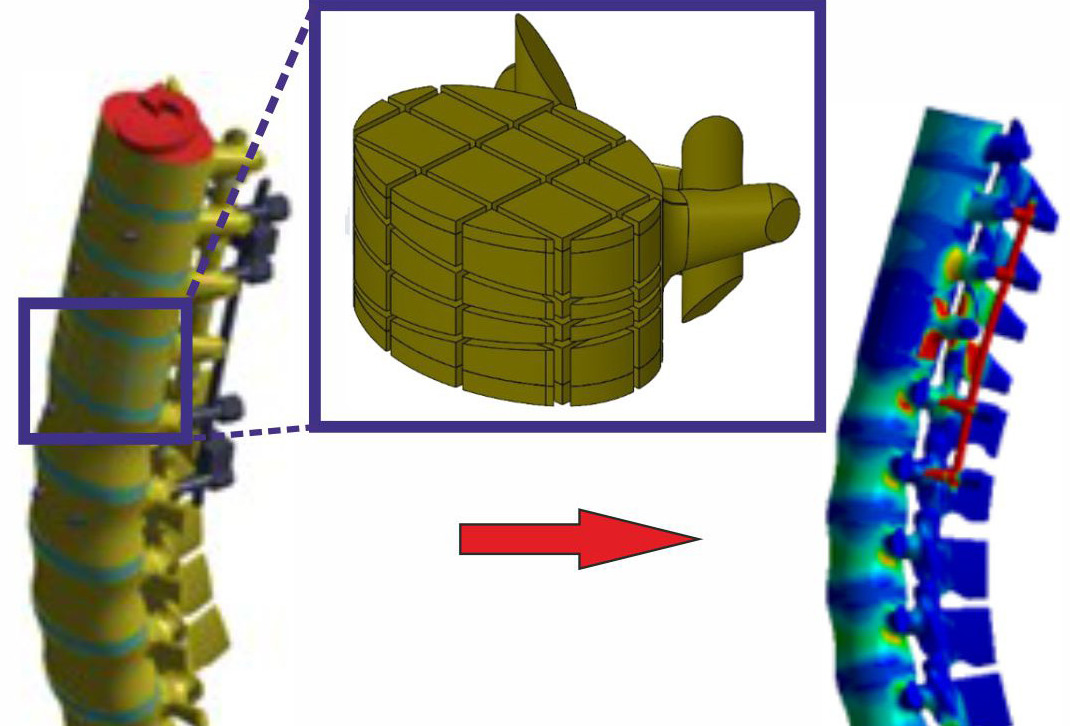
Objective: To examine the stress-strain state of the thoracolumbar spine model with a burst fracture of the Th12 vertebra under various transpedicular fixation options influenced by rotational loading.
Materials and Methods: A mathematical finite-element model of the human thoracolumbar spine was developed, including a burst fracture of the Th12 vertebra and a transpedicular stabilization system containing eight screws implanted in the Th10, Th11, L1, and L2 vertebrae. Four variants of transpedicular fixation were modelled using short and long screws passing through the anterior surface of the vertebra, with and without two crosslinks.
Results: The analysis showed sufficiently high loading values for both the bone structures of the models and the elements of the metal construct. The maximum stress level in the body of the damaged vertebra was 33.2, 26.7, 30.1, and 24.2 MPa, respectively, for models with monocortical screws without crosslinks, bicortical screws without crosslinks, monocortical screws with crosslinks, and bicortical screws with crosslinks. High values were also recorded for the vertebrae adjacent to the damaged one: 13.0, 8.4, 10.9, and 7.1 MPa for the L1 vertebra and 10.2, 8.9, 7.1, and 6.2 MPa for the Th11 vertebra in the respective models. The stress on the supporting rods was registered at 582.0, 512.5, 512.6, and 452.7 MPa respectively.
Conclusion: The conducted analysis demonstrated that under rotational loading, the model with monocortical screws without crosslinks shows the highest peak loads at control points, whereas the model with bicortical screws and crosslinks shows the minimum. Meanwhile, models with short screws and crosslinks and long screws without crosslinks exhibit comparable results
References
- Fradet, L., Petit, Y., Wagnac, E., Aubin, C.-E., Arnoux, P.-J. (2013). Biomechanics of thoracolumbar junction vertebral fractures from various kinematic conditions. Medical & Biological Engineering & Computing, 52 (1), 87–94. https://doi.org/10.1007/s11517-013-1124-8
- Qiu, T.-X., Tan, K.-W., Lee, V.-S., Teo, E.-C. (2006). Investigation of thoracolumbar T12–L1 burst fracture mechanism using finite element method. Medical Engineering & Physics, 28 (7), 656–664. https://doi.org/10.1016/j.medengphy.2005.10.011
- Wang, H., Zhang, Y., Xiang, Q., Wang, X., Li, C., Xiong, H., Zhou, Y. (2012). Epidemiology of traumatic spinal fractures: experience from medical university–affiliated hospitals in Chongqing, China, 2001–2010. Journal of Neurosurgery: Spine, 17 (5), 459–468. https://doi.org/10.3171/2012.8.spine111003
- Rajasekaran, S., Kanna, R. M., Shetty, A. P. (2015). Management of thoracolumbar spine trauma. Indian Journal of Orthopaedics, 49 (1), 72–82. https://doi.org/10.4103/0019-5413.143914
- Verlaan, J. J., Diekerhof, C. H., Buskens, E., van der Tweel, I., Verbout, A. J., Dhert, W. J. A., Oner, F. C. (2004). Surgical Treatment of Traumatic Fractures of the Thoracic and Lumbar Spine. Spine, 29 (7), 803–814. https://doi.org/10.1097/01.brs.0000116990.31984.a9
- Sasani, M., Özer, A. F. (2009). Single-Stage Posterior Corpectomy and Expandable Cage Placement for Treatment of Thoracic or Lumbar Burst Fractures. Spine, 34 (1), E33–E40. https://doi.org/10.1097/brs.0b013e318189fcfd
- Roy-Camille, R., Saillant, G., Mazel, C. (1986). Internal Fixation of the Lumbar Spine with Pedicle Screw Plating. Clinical Orthopaedics and Related Research, 203, 7–17. https://doi.org/10.1097/00003086-198602000-00003
- Harrington, P. R. (1973). The History and Development of Harrington Instrumentation. Clinical Orthopaedics and Related Research, 93, 110–112. https://doi.org/10.1097/00003086-197306000-00013
- Tanasansomboon, T., Kittipibul, T., Limthongkul, W., Yingsakmongkol, W., Kotheeranurak, V., Singhatanadgige, W. (2022). Thoracolumbar Burst Fracture without Neurological Deficit: Review of Controversies and Current Evidence of Treatment. World Neurosurgery, 162, 29–35. https://doi.org/10.1016/j.wneu.2022.03.061
- Chan, B. C. F., Craven, B. C., Furlan, J. C. (2018). A scoping review on health economics in neurosurgery for acute spine trauma. Neurosurg Focus, 44 (5), E15. http://doi.org/10.3171/2018.2.Focus17778
- Assaker, R. (2004). Minimal access spinal technologies: state-of-the-art, indications, and techniques. Joint Bone Spine, 71 (6), 459–469. https://doi.org/10.1016/j.jbspin.2004.08.006
- Walker, C. T., Xu, D. S., Godzik, J., Turner, J. D., Uribe, J. S., Smith, W. D. (2018). Minimally invasive surgery for thoracolumbar spinal trauma. Annals of Translational Medicine, 6 (6), 102–102. https://doi.org/10.21037/atm.2018.02.10
- Dong, S., Li, Z., Tang, Z., Zheng, Y., Yang, H., Zeng, Q. (2022). Predictors of adverse events after percutaneous pedicle screws fixation in patients with single-segment thoracolumbar burst fractures. BMC Musculoskeletal Disorders, 23 (1). https://doi.org/10.1186/s12891-022-05122-1
- Karami, K. J., Buckenmeyer, L. E., Kiapour, A. M., Kelkar, P. S., Goel, V. K., Demetropoulos, C. K., Soo, T. M. (2015). Biomechanical Evaluation of the Pedicle Screw Insertion Depth Effect on Screw Stability Under Cyclic Loading and Subsequent Pullout. Journal of Spinal Disorders & Techniques, 28 (3), E133–E139. https://doi.org/10.1097/bsd.0000000000000178
- Burkhard, M. D., Cornaz, F., Spirig, J. M., Wanivenhaus, F., Loucas, R., Fasser, M.-R., Widmer, J., Farshad, M. (2021). Posterior spinal instrumentation and decompression with or without cross-link? North American Spine Society Journal (NASSJ), 8, 100093. https://doi.org/10.1016/j.xnsj.2021.100093
- Nekhlopochyn, O. S., Verbov, V. V., Cheshuk, I. V., Vorodi, M. V., Karpinsky, M. Yu., Yaresko, O. V. (2023). The biomechanical state of the thoracolumbar junction with various options of transpedicular fixation under flexion load. Ukrainian Neurosurgical Journal, 29 (2), 49–56. https://doi.org/10.25305/unj.277152
- Nekhlopochyn, O. S., Verbov, V. V., Karpinsky, M. Yu., Yaresko, O. V. (2021). Biomechanical evaluation of the pedicle screw insertion depth and role of cross-link in thoracolumbar junction fracture surgery: a finite element study under compressive loads. Ukrainian Neurosurgical Journal, 27 (3), 25–32. https://doi.org/10.25305/unj.230621
- Boccaccio, A., Pappalettere, C.; Klika, V. (Ed.) (2011). Mechanobiology of Fracture Healing: Basic Principles and Applications in Orthodontics and Orthopaedics. Theoretical Biomechanics. Croatia: InTech, 21–48. https://doi.org/10.5772/19420
- Cowin, S. C. (2001). Bone Mechanics Handbook. Boca Raton: CRC Press, 980.
- International Organization for Standardization (2021). ISO 5832-3:2021: Implants for Surgery: Metallic Materials. Wrought titanium 6-aluminium 4-vanadium alloy. Part 3. Geneva: ISO, 17
- Rao, S. S. (2005) The Finite Element Method in Engineering. Elsevier Science, 663.
- Kurowski, P. M. (2007). Engineering Analysis with COSMOSWorks 2007. SDC Publications, 263
- Nekhlopochyn, O. S., Verbov, V. V., Cheshuk, I. V., Karpinsky, M. Yu., Yaresko, O. V. (2023). Biomechanical characteristics of thoracolumbar junction under rotational loading after decompression-stabilization surgery. Bulletin of Problems Biology and Medicine, 1 (3), 233–244. https://doi.org/10.29254/2077-4214-2023-3-170-233-244
- Panjabi, M. M., Oxland, T. R., Lin, R. M., McGowen, T. W. (1994). Thoracolumbar burst fracture. A biomechanical investigation of its multidirectional flexibility. Spine, 19 (5), 578–585. https://doi.org/10.1097/00007632-199403000-00014
- Niinomi, M. (2008). Mechanical biocompatibilities of titanium alloys for biomedical applications. Journal of the Mechanical Behavior of Biomedical Materials, 1 (1), 30–42. https://doi.org/10.1016/j.jmbbm.2007.07.001
- Mohi Eldin, M. M., Ali, A. M. A. (2014). Lumbar Transpedicular Implant Failure: A Clinical and Surgical Challenge and Its Radiological Assessment. Asian Spine Journal, 8 (3), 281–279. https://doi.org/10.4184/asj.2014.8.3.281
- Galbusera, F., Volkheimer, D., Reitmaier, S., Berger-Roscher, N., Kienle, A., Wilke, H.-J. (2015). Pedicle screw loosening: a clinically relevant complication? European Spine Journal, 24 (5), 1005–1016. https://doi.org/10.1007/s00586-015-3768-6
- Chen, C.-S., Chen, W.-J., Cheng, C.-K., Jao, S.-H. E., Chueh, S.-C., Wang, C.-C. (2005). Failure analysis of broken pedicle screws on spinal instrumentation. Medical Engineering & Physics, 27 (6), 487–496. https://doi.org/10.1016/j.medengphy.2004.12.007
- Alkosha, H. M., Omar, S. A., Albayar, A., Awad, B. I. (2019). Candidates for Percutaneous Screw Fixation Without Fusion in Thoracolumbar Fractures: A Retrospective Matched Cohort Study. Global Spine Journal, 10 (8), 982–991. https://doi.org/10.1177/2192568219886320
- Vaccaro, A. R., Lehman, R. A., Hurlbert, R. J., Anderson, P. A., Harris, M., Hedlund, R. et al. (2005). A New Classification of Thoracolumbar Injuries. Spine, 30 (20), 2325–2333. https://doi.org/10.1097/01.brs.0000182986.43345.cb
- Moon, M.-S., Yu, C. G., Jeon, J. M., Wi, S. M. (2023). Usefulness of Percutaneous Pedicle Screw Fixation for Treatment of Lower Lumbar Burst (A3-A4) Fractures: Comparative Study with Thoracolumbar Junction Fractures. Indian Journal of Orthopaedics, 57 (9), 1415–1422. https://doi.org/10.1007/s43465-023-00911-9
- Krag, M. H., Beynnon, B. D., Pope, M. H., DeCoster, T. A. (1988). Depth of Insertion of Transpedicular Vertebral Screws into Human Vertebrae. Journal of Spinal Disorders, 1 (4), 287–294. https://doi.org/10.1097/00002517-198800140-00002
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Oleksii Nekhlopochyn, Vadim Verbov, Ievgen Cheshuk, Mykhailo Karpinsky, Olexander Yaresko

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








