Prognostic significance of catestatin in patients with primary hypertension and type 2 diabetes mellitus
DOI:
https://doi.org/10.15587/2519-4798.2023.291591Keywords:
primary hypertension, type 2 diabetes mellitus, major adverse cardiovascular events, catestatin, relaxin-2, biomarkerAbstract
The aim of this study was to determine predictors of cardiovascular complications of arterial hypertension (AH) and type 2 diabetes mellitus (T2DM) and investigate the prognostic potential of catestatin (CST) and relaxin-2 (RLN-2) in this patient population.
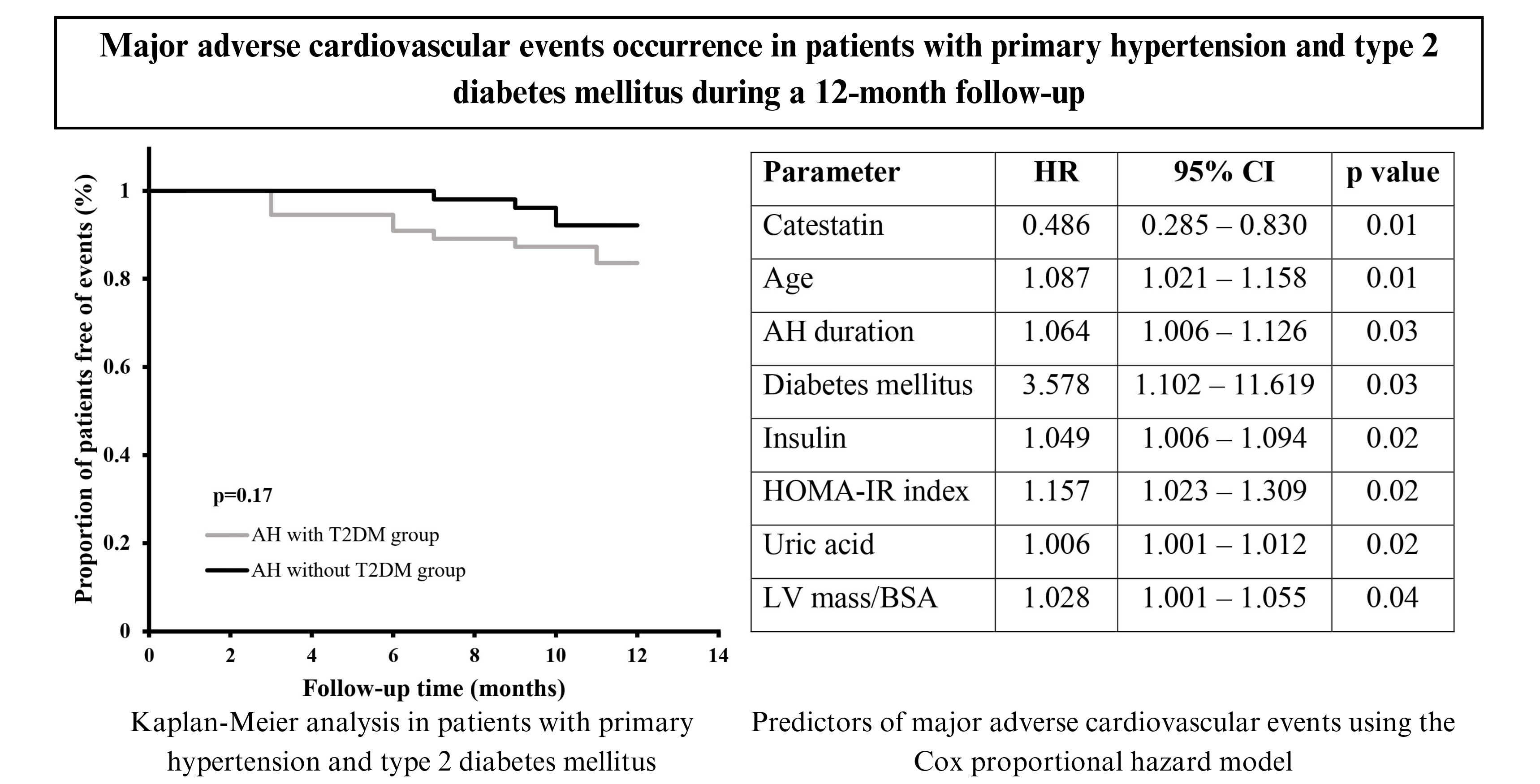
Materials and methods. The research was performed in accordance with all ethical principles of the Declaration of Helsinki. All study participants signed a written informed consent. This study involved 106 patients with primary hypertension and 30 healthy volunteers. 55 hypertensive patients had comorbid T2DM. Plasma CST and RLN-2 levels were measured by an enzyme-linked immunosorbent assay. Major adverse cardiovascular events (MACE) were collected during 12-month follow-up via telephone interviews at visits in months 3, 6, 9, and 12. The end points of this study were acute myocardial infarction, ischemic stroke, acute heart failure and cardiac death. Statistical data analysis was performed using the SPSS 25.0 statistical software.
Results. 13 end-points were registered in patients with AH during the 12-month follow-up period, but the difference in frequency of MACE occurrence between patients with AH and T2DM and hypertensive patients without T2DM was insignificant (p=0.181). The Cox proportional hazard model indicated CST (p=0.01), but not RLN-2 (p=0.20), as an independent predictor of MACE in hypertensive patients. Age (p=0.01), AH duration (p=0.03), presence of T2DM (p=0.03), HOMA-IR index (p=0.02), insulin (p=0.02) and uric acid levels (p=0.02) were also established as independent factors of end-points occurrence.
Conclusions. CST is an independent factor for predicting cardiovascular complications of AH, which allows us to consider it as a prognostic biomarker in patients with AH, especially hypertensive patients with comorbidity T2DM
References
- World Heart Report 2023: Confronting the World’s Number One Killer (2023). World Heart Federation. Geneva, 48. Available at: https://world-heart-federation.org/wp-content/uploads/World-Heart-Report-2023.pdf Last accessed: 25.11.2023
- Lindstrom, M., DeCleene, N., Dorsey, H., Fuster, V., Johnson, C. O., LeGrand, K. E. et al. (2022). Global Burden of Cardiovascular Diseases and Risks Collaboration, 1990-2021. Journal of the American College of Cardiology, 80 (25), 2372–2425. doi: https://doi.org/10.1016/j.jacc.2022.11.001
- Ma, J., Chen, X. (2022). Advances in pathogenesis and treatment of essential hypertension. Frontiers in Cardiovascular Medicine, 9. doi: https://doi.org/10.3389/fcvm.2022.1003852
- Di Palo, K. E., Barone, N. J. (2022). Hypertension and Heart Failure. Cardiology Clinics, 40 (2), 237–244. doi: https://doi.org/10.1016/j.ccl.2021.12.011
- Bozic, J., Kumric, M., Ticinovic Kurir, T., Urlic, H., Martinovic, D., Vilovic, M. et al. (2021). Catestatin as a Biomarker of Cardiovascular Diseases: A Clinical Perspective. Biomedicines, 9 (12), 1757. doi: https://doi.org/10.3390/biomedicines9121757
- Aragón-Herrera, A., Feijóo-Bandín, S., Anido-Varela, L., Moraña-Fernández, S., Roselló-Lletí, E., Portolés, M. et al. (2022). Relaxin-2 as a Potential Biomarker in Cardiovascular Diseases. Journal of Personalized Medicine, 12 (7), 1021. doi: https://doi.org/10.3390/jpm12071021
- Pankova, O., Korzh, O. (2023). Plasma catestatin levels are related to metabolic parameters in patients with essential hypertension and type 2 diabetes mellitus. Heart and Vessels. doi: https://doi.org/10.1007/s00380-023-02318-w
- Lang, R. M., Badano, L. P., Mor-Avi, V., Afilalo, J., Armstrong, A., Ernande, L. et al. (2015). Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Journal of the American Society of Echocardiography, 28 (1), 1-39.e14. doi: https://doi.org/10.1016/j.echo.2014.10.003
- Kumric, M., Vrdoljak, J., Dujic, G., Supe-Domic, D., Ticinovic Kurir, T., Dujic, Z., Bozic, J. (2022). Serum Catestatin Levels Correlate with Ambulatory Blood Pressure and Indices of Arterial Stiffness in Patients with Primary Hypertension. Biomolecules, 12 (9), 1204. doi: https://doi.org/10.3390/biom12091204
- Durakoglugil, M. E., Ayaz, T., Kocaman, S. A., Kirbas, A., Durakoglugil, T., Erdogan, T. et al. (2015). The relationship of plasma catestatin concentrations with metabolic and vascular parameters in untreated hypertensive patients: Influence on high-density lipoprotein cholesterol. The Anatolian Journal of Cardiology, 15 (7), 577–585. doi: https://doi.org/10.5152/akd.2014.5536
- Gedikli, O., Yilmaz, H., Kiris, A., Karaman, K., Ozturk, S., Baykan, M., Ucar, U., Durmus, I., Karahan, C., Celik, S. (2009). Circulating levels of relaxin and its relation to cardiovascular function in patients with hypertension. Blood Pressure, 18 (1-2), 68–73. doi: https://doi.org/10.1080/08037050902864086
- Sanidas, E., Tsakalis, K., Papadopoulos, D. P., Zerva, K., Velliou, M., Perrea, D. et al. (2018). The impact of apelin and relaxin plasma levels in masked hypertension and white coat hypertension. The Journal of Clinical Hypertension, 21 (1), 48–52. doi: https://doi.org/10.1111/jch.13449
- Zhu, D., Xie, H., Wang, X., Liang, Y., Yu, H., Gao, W. (2015). Correlation of Plasma Catestatin Level and the Prognosis of Patients with Acute Myocardial Infarction. PLOS ONE, 10 (4), e0122993. doi: https://doi.org/10.1371/journal.pone.0122993
- Xu, W., Yu, H., Wu, H., Li, S., Chen, B., Gao, W. (2016). Plasma Catestatin in Patients with Acute Coronary Syndrome. Cardiology, 136 (3), 164–169. doi: https://doi.org/10.1159/000448987
- Peng, F., Chu, S., Ding, W., Liu, L., Zhao, J., Cui, X. et al. (2016). The predictive value of plasma catestatin for all-cause and cardiac deaths in chronic heart failure patients. Peptides, 86, 112–117. doi: https://doi.org/10.1016/j.peptides.2016.10.007
- Wołowiec, Ł., Rogowicz, D., Banach, J., Gilewski, W., Sinkiewicz, W., Grześk, G. (2020). Catestatin as a New Prognostic Marker in Stable Patients with Heart Failure with Reduced Ejection Fraction in Two-Year Follow-Up. Disease Markers, 2020, 1–10. doi: https://doi.org/10.1155/2020/8847211
- Miró, Ò., Herrero-Puente, P., Prieto, B., García-García, M., García-Hernández, P., Martín-Sánchez, F. J. et al. (2018). The subset of patients with acute heart failure able to secrete relaxin-2 at pregnancy concentrations could have a longer survival: a pilot study. Biomarkers, 23 (6), 573–579. doi: https://doi.org/10.1080/1354750x.2018.1463564
- Zhou, H., Qu, X., Gao, Z., Zheng, G., Lin, J., Su, L. et al. (2016). Relaxin Level in Patients With Atrial Fibrillation and Association with Heart Failure Occurrence. Medicine, 95 (21), e3664. doi: https://doi.org/10.1097/md.0000000000003664
- Qu, X., Chen, L., Sun, L., Chen, C., Gao, Z., Huang, W., Zhou, H. (2019). Serum relaxin level predicts recurrence of atrial fibrillation after radiofrequency catheter ablation. Heart and Vessels, 34 (9), 1543–1551. doi: https://doi.org/10.1007/s00380-019-01386-1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Olena Pankova, Oleksii Korzh

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








