Assessment of the implantation window and embryonic factor impact to the treatment of recurrent implantation failure (RIF). A prospective study
DOI:
https://doi.org/10.15587/2519-4798.2024.296672Keywords:
implantation window (IW), pipelle biopsy, implantation failure, preimplantation genetic testing (PGT), in vitro fertilization (IVF)Abstract
The aim: to study of the prognostic value of endometrial receptivity and preimplantation genetic diagnosis of embryos, and their influence on the effectiveness of in vitro fertilization (IVF) programs. We also evaluate the importance of this factor in comparison with other potential causes of infertility.
Materials and methods: This prospective cohort study included 123 infertile women who underwent in vitro fertilization (IVF) treatment. 93 patients had repeated unsuccessful implantation attempts and were divided into three groups: group 1 - patients who were treated using genetically untested embryos according to a standard fixed stimulation protocol, group 2 - patients who were treated using euploid embryos after preimplantation genetic screening according to standard fixed protocol; group 3 - patients who underwent treatment using euploid embryos after pre-implantation genetic screening and determination of the implantation window with subsequent modification of the stimulation protocol, according to the endometrial examination result. 30 patients had a first attempt at IVF, which was carried out using genetically untested embryos, according to a standard fixed protocol, and made up the control group (CG).
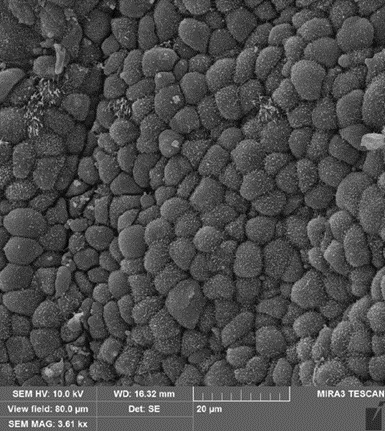
Determination of the window of implantation was carried out by triple aspiration biopsy of the endometrium during the luteal phase of the menstrual cycle since the endometrium is most susceptible to implantation during this period. Samples were analyzed using scanning electron microscopy. Based on the results obtained, the endometrial preparation protocol was individualized for the next attempt. preimplantation genetic testing (PGT) of embryos was carried out by the next generation (NGS) method.
Statistical analysis was performed using IBM SPSS V25.0 for Windows software.
Results: According to the obtained results, patient characteristics, screening rates, IVF cycle characteristics, and the number, quality, and stage of transferred embryos were compared between groups. The rate of clinical pregnancy was 46.7 % among patients of group 1.70 % among patients of group 2, 82.8 % among patients of group 3 and 50.0 % of the control group and statistically significantly different between groups (χ2=10.955, p= 0.012). The rate of live birth was 43.3 % among patients of group 1, 53.3 % among patients of group 2, 72.4 % among patients of group 3 and 43.3 % - of the control group, however, it did not differ statistically significantly between groups (χ2=6,639, р=0,084)
Conclusions: The unique window of implantation and the embryonic factor are among the main reasons for multiple failed implantation attempts. Personalization of the endometrial preparation protocol and preimplantation embryo diagnosis are effective methods to improve IVF outcomes
References
- De Geyter, C., Calhaz-Jorge, C., Kupka, M. S., Wyns, C., Mocanu, E., Motrenko, T., Scaravelli, G., Smeenk, J., Vidakovic, S., Goossens, V. (2020). Corrigendum. ART in Europe, 2015: results generated from European registries by ESHRE. Human Reproduction Open, 2020 (3). https://doi.org/10.1093/hropen/hoaa038
- Jones, H. W. Jr., Oehninger, S., Bocca, S., Stadtmauer, L., Mayer, J. (2010). Reproductive efficiency of human oocytes fertilized in vitro. Facts Views Vis Obgyn, 2 (3), 169–171.
- Edwards, R. G. (1994). Implantation, interception and contraception. Human Reproduction, 9 (6), 985–995. https://doi.org/10.1093/oxfordjournals.humrep.a138673
- Craciunas, L., Gallos, I., Chu, J., Bourne, T., Quenby, S., Brosens, J. J., Coomarasamy, A. (2019). Conventional and modern markers of endometrial receptivity: a systematic review and meta-analysis. Human Reproduction Update, 25 (2), 202–223. https://doi.org/10.1093/humupd/dmy044
- Lessey, B. A., Young, S. L. (2019). What exactly is endometrial receptivity? Fertility and Sterility, 111(4), 611–617. https://doi.org/10.1016/j.fertnstert.2019.02.009
- Noyes, R. W., Hertig, A. T., Rock, J. (1950). Dating the Endometrial Biopsy. Fertility and Sterility, 1 (1), 3–25. https://doi.org/10.1016/s0015-0282(16)30062-0
- Nikas, G., Drakakis, P., Loutradis, D., Mara-Skoufari, C., Koumantakis, E., Michalas, S., Psychoyos, A. (1995). Implantation: Uterine pinopodes as markers of the ‘nidation window’ in cycling women receiving exogenous oestradiol and progesterone. Human Reproduction, 10 (5), 1208–1213. https://doi.org/10.1093/oxfordjournals.humrep.a136120
- Martel, D., Frydman, R., Glissant, M., Maggioni, C., Roche, D., Psychoyos, A. (1987). Scanning electron microscopy of postovulatory human endometrium in spontaneous cycles and cycles stimulated by hormone treatment. Journal of Endocrinology, 114 (2), 319–324. https://doi.org/10.1677/joe.0.1140319
- Lopata, A., Bentin-Ley, U., Enders, A. (2002). Pinopodes and implantation. Reviews in Endocrine and Metabolic Disorders, 3 (2), 77–86. https://doi.org/10.1023/a:1015455709833
- Forman, E. J., Tao, X., Ferry, K. M., Taylor, D., Treff, N. R., Scott, R. T. (2012). Single embryo transfer with comprehensive chromosome screening results in improved ongoing pregnancy rates and decreased miscarriage rates. Human Reproduction, 27 (4), 1217–1222. https://doi.org/10.1093/humrep/des020
- Takeuchi, K. (2020). Pre‐implantation genetic testing: Past, present, future. Reproductive Medicine and Biology, 20 (1), 27–40. https://doi.org/10.1002/rmb2.12352
- Amin, J., Patel, R., JayeshAmin, G., Gomedhikam, J., Surakala, S., Kota, M. (2022). Personalized Embryo Transfer Outcomes in Recurrent Implantation Failure Patients Following Endometrial Receptivity Array With Pre-Implantation Genetic Testing. Cureus. https://doi.org/10.7759/cureus.26248
- Cozzolino, M., Diaz-Gimeno, P., Pellicer, A., Garrido, N. (2020). Evaluation of the endometrial receptivity assay and the preimplantation genetic test for aneuploidy in overcoming recurrent implantation failure. Journal of Assisted Reproduction and Genetics, 37 (12), 2989–2997. https://doi.org/10.1007/s10815-020-01948-7
- Alpha Scientists in Reproductive Medicine, & ESHRE Special Interest Group Embryology (2011). Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Reproductive BioMedicine Online, 22 (6), 632–646. https://doi.org/10.1016/j.rbmo.2011.02.001
- Gallos, I. D., Khairy, M., Chu, J., Rajkhowa, M., Tobias, A., Campbell, A., Dowell, K., Fishel, S., Coomarasamy, A. (2018). Optimal endometrial thickness to maximize live births and minimize pregnancy losses: Analysis of 25,767 fresh embryo transfers. Reproductive BioMedicine Online, 37 (5), 542–548. https://doi.org/10.1016/j.rbmo.2018.08.025
- Swierkowski-Blanchard, N., Boitrelle, F., Alter, L., Selva, J., Quibel, T., Torre, A. (2017). Uterine contractility and elastography as prognostic factors for pregnancy after intrauterine insemination. Fertility and Sterility, 107 (4), 961-968.e3. https://doi.org/10.1016/j.fertnstert.2017.02.002
- Chung, C. H. S., Wong, A. W. Y., Chan, C. P. S., Saravelos, S. H., Kong, G. W. S., Cheung, L. P. et al. (2017). The changing pattern of uterine contractions before and after fresh embryo transfer and its relation to clinical outcome. Reproductive BioMedicine Online, 34 (3), 240–247. https://doi.org/10.1016/j.rbmo.2016.12.011
- Simon, C., Gomez, C., Cabanillas, S., Vladimirov, I. K., Castillon, G., Giles, J. et al. (2019). In vitro fertilization with personalized blastocyst transfer versus frozen or fresh blastocyst transfer: a multicenter, randomized clinical trial. Fertility and Sterility, 112 (3), e56–e57. https://doi.org/10.1016/j.fertnstert.2019.07.273
- Florio, P., Bruni, L., Galleri, L., Reis, F. M., Borges, L. E., Bocchi, C. et al. (2010). Evaluation of endometrial activin A secretion for prediction of pregnancy after intrauterine insemination. Fertility and Sterility, 93 (7), 2316–2320. https://doi.org/10.1016/j.fertnstert.2008.12.125
- Rahiminejad, M. E., Moaddab, A., Ganji, M., Eskandari, N., Yepez, M., Rabiee, S., Wise, M., Ruano, R., Ranjbar, A. (2016). Oxidative stress biomarkers in endometrial secretions: A comparison between successful and unsuccessful in vitro fertilization cycles. Journal of Reproductive Immunology, 116, 70–75. https://doi.org/10.1016/j.jri.2016.05.003
- Santi, A., Felser, R., Bersinger, N. A., Wunder, D. M., McKinnon, B., Mueller, M. D. (2011). The hysteroscopic view of infertility: the mid-secretory endometrium and treatment success towards pregnancy. Gynecological Surgery, 9 (2), 147–150. https://doi.org/10.1007/s10397-011-0687-3
- Kragh, M. F., Karstoft, H. (2021). Embryo selection with artificial intelligence: how to evaluate and compare methods? Journal of Assisted Reproduction and Genetics, 38 (7), 1675–1689. https://doi.org/10.1007/s10815-021-02254-6
- Bori, L., Paya, E., Alegre, L., Viloria, T. A., Remohi, J. A., Naranjo, V., Meseguer, M. (2020). Novel and conventional embryo parameters as input data for artificial neural networks: an artificial intelligence model applied for prediction of the implantation potential. Fertility and Sterility, 114 (6), 1232–1241. https://doi.org/10.1016/j.fertnstert.2020.08.023
- Chen, S. (2022). Chinese scientists create AI nanny to look after embryos in artificial womb. Available at: https://www.scmp.com/news/china/science/article/3165325/chinese-scientists-create-ai-nanny-look-after-babies-artificial
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Oleksandra Kozyra, Mykhailo Medvediev

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








