The relationship of dyslipidemia and insulin resistance in patients with type 2 diabetes and the metabolic syndrome
DOI:
https://doi.org/10.15587/2519-4798.2023.297369Keywords:
type 2 diabetes, metabolic syndrome, insulin resistance, obesity, non-alcoholic fatty liver disease, non-alcoholic steatohepatosis, dyslipidemia, glycemic control in patients with type 2 diabetes with MSAbstract
The aim of the research was to study the relationship between dyslipidemia and insulin resistance in patients with type 2 diabetes with metabolic syndrome.
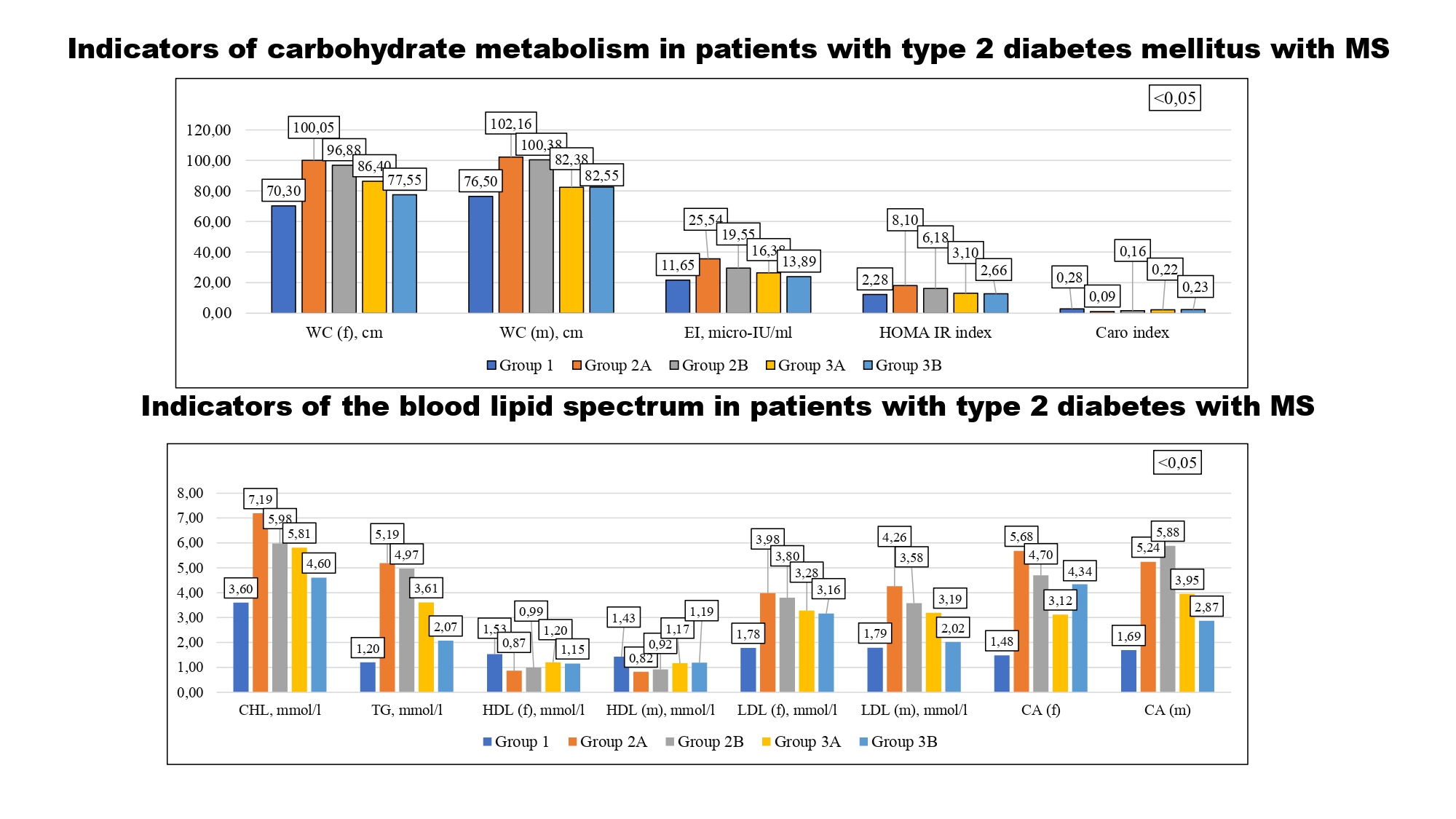
Materials and methods: In accordance with the aim and objectives of the study, the group of subjects consisted of 120 patients with type 2 diabetes mellitus with MS who were undergoing inpatient treatment in the endocrinology department of the KNP "Regional Clinical Hospital of the Ivano-Frankivsk Regional Council" and 15 practically healthy individuals (PHI), who made up the control group. The degree of IR was determined by waist circumference (WC), IR indices: the HOMA-IR index and the Caro index. The distribution of patients with type 2 diabetes mellitus with MS and without signs of MS was carried out, depending on the presence of NASH. The concentration of endogenous insulin (EI) was determined by the enzyme immunoassay method using an autonomous chemiluminescence analyzer Maglumi 800 with a set of reagents Maglumi "Insulin" Shanghai International Holding Corp. GmbH (Europe), Hamburg, Germany. Glycated hemoglobin (HbA1c) was determined using the "Glycosylated Hemoglobin Spl" reagent of Granum Laboratory LLC, Kharkiv, Ukraine, using a ULAB 108UV spectrophotometer. The level of triglycerides and HDL-CHD in blood serum was determined with the help of the "Cholesterol Spl" reagent of the "Granum Laboratory" LLC, Ukraine, Kharkiv, using the ER 500 enzyme immunoassay analyzer.
Results: calculation of generally accepted indices of insulin resistance, in particular the HOMA IR index, OT, BMI indicate the presence of significant insulin resistance in patients with type 2 diabetes with MS, while the changes were the greatest in patients with type 2 diabetes with MS and NASH. Insulin resistance syndrome contributes to lipid imbalance and is a metabolic prerequisite for the development of NASH.
Conclusions. The results of the study are recommended for practical use in health care: correction of dyslipidemia against the background of glycemic control
References
- Ambachew, S., Endalamaw, A., Worede, A., Tegegne, Y., Melku, M., Biadgo, B. (2020). The Prevalence of Metabolic Syndrome in Ethiopian Population: A Systematic Review and Meta-analysis. Journal of Obesity, 2020, 1–14. doi: https://doi.org/10.1155/2020/2701309
- Charlton, M. R., Burns, J. M., Pedersen, R. A., Watt, K. D., Heimbach, J. K., Dierkhising, R. A. (2011). Frequency and Outcomes of Liver Transplantation for Nonalcoholic Steatohepatitis in the United States. Gastroenterology, 141 (4), 1249–1253. doi: https://doi.org/10.1053/j.gastro.2011.06.061
- Cotter, T. G., Rinella, M. (2020). Nonalcoholic Fatty Liver Disease 2020: The State of the Disease. Gastroenterology, 158 (7), 1851–1864. doi: https://doi.org/10.1053/j.gastro.2020.01.052
- Ekstedt, M., Franzén, L. E., Mathiesen, U. L., Thorelius, L., Holmqvist, M., Bodemar, G., Kechagias, S. (2006). Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology, 44 (4), 865–873. doi: https://doi.org/10.1002/hep.21327
- Ertle, J., Dechêne, A., Sowa, J., Penndorf, V., Herzer, K., Kaiser, G. et al. (2011). Non‐alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. International Journal of Cancer, 128 (10), 2436–2443. doi: https://doi.org/10.1002/ijc.25797
- Ford, E. S., Giles, W. H., Dietz, W. H. (2002). Prevalence of metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA, 287 (3), 356–359. doi: https://doi.org/10.1001/jama.287.3.356
- Knebel, B., Fahlbusch, P., Dille, M., Wahlers, N., Hartwig, S., Jacob, S. et al. (2019). Fatty Liver Due to Increased de novo Lipogenesis: Alterations in the Hepatic Peroxisomal Proteome. Frontiers in Cell and Developmental Biology, 7. doi: https://doi.org/10.3389/fcell.2019.00248
- Liashuk, R. P., Liashuk, P. M., Hluhovska, S. V. (2015). Comorbidity of metabolic syndrome and sleep apnea. Bukovinian Medical Herald, 19 (3 (75)), 273–275. doi: https://doi.org/10.24061/2413-0737.xix.3.75.2015.192
- Parthasarathy, G., Revelo, X., Malhi, H. (2020). Pathogenesis of Nonalcoholic Steatohepatitis: An Overview. Hepatology Communications, 4 (4), 478–492. doi: https://doi.org/10.1002/hep4.1479
- Younossi, Z. M. (2019). Non-alcoholic fatty liver disease – A global public health perspective. Journal of Hepatology, 70 (3), 531–544. doi: https://doi.org/10.1016/j.jhep.2018.10.033
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Taras Romaniv, Nadiya Skrypnyk

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








