Acute pain syndromes in injuries to the nerves and plexuses of the limbs
DOI:
https://doi.org/10.15587/2519-4798.2024.299496Keywords:
pain, pain syndrome, neuropathic pain, nociceptive pain, injuries to nerves and plexuses of the limbs, neuropathies and plexopathies, treatment of neuropathic pain syndromeAbstract
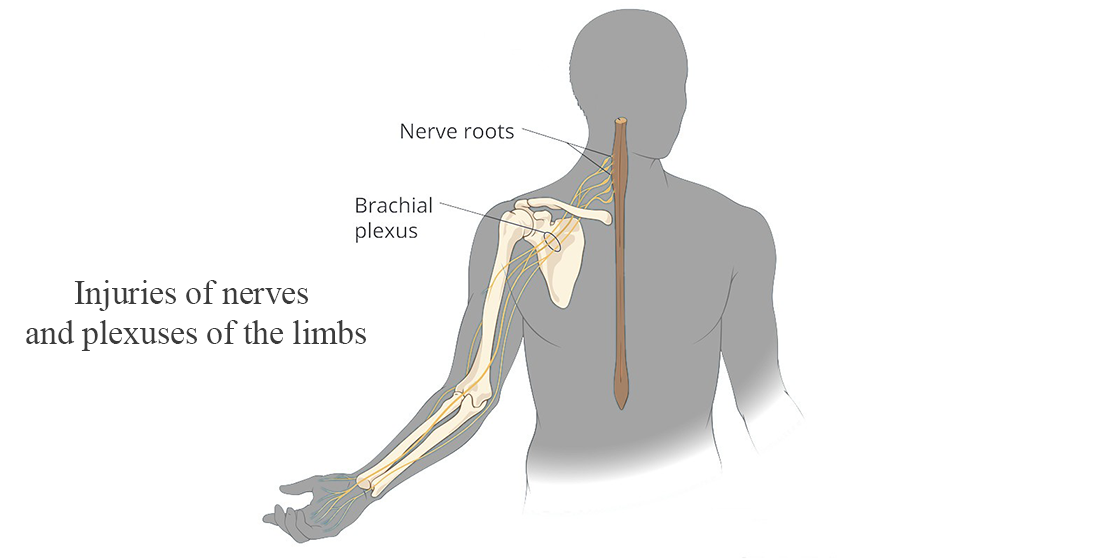
Injuries of peripheral nerves and plexuses cause serious disorders in the affected limbs. Unfortunately, the frequency of nerve injuries and limb plexuses is steadily increasing in our country, due to hostilities, which emphasizes the extreme relevance of this pathology.
The aim of the review is to consider the current data on pathophysiological mechanisms, clinical manifestations, and treatment of acute pain syndromes in patients with injuries of peripheral nerves and limb plexuses.
Materials and methods. Scientific databases PubMed, Google Scholar, Scopus, Cochrane Library, as well as the materials of the International Association for the study of pain were used to search for sources of research information. The main studies were found in Pubmed, Google Scholar and materials of the International Association for the study of pain and made up 191 sources of information, 150 of which were excluded from the review due to insufficient data on pathophysiological mechanisms, clinical manifestations, and treatment of pain syndromes in patients with damage to the nerves and plexuses of the limbs, thus 41 sources of information formed the basis of the review.
Results: Brachial plexus and peripheral nerve injuries can be associated with any combination of nociceptive, neuropathic, phantom limb pain, and even complex regional pain syndromes. Acute neuropathic pain is an under-recognized condition, often difficult to treat and can progress to persistent pain and disability. Neuropathic pain develops because the main damage affects the somatosensory system. It is caused by peripheral nerve damage and associated changes in the central nervous system. The first line of pharmacological treatment for neuropathic pain according to current guidelines is anticonvulsant drugs that affect neuronal calcium channels, as well as tri- and tetracyclic antidepressants and selective serotonin/norepinephrine reuptake inhibitors.
Conclusions: At the current stage, progress has been made in understanding the mechanisms of development of the pathological condition and in the development of therapeutic approaches, however, the chronicity of pain syndrome in patients with damage to the nerves and plexuses of the limbs is still high, which requires further research to develop complex pathogenetic therapy and better understanding of the mechanisms pain in this category of patients
References
- Teixeira, M. J., da Paz, M. G. da S., Bina, M. T., Santos, S. N., Raicher, I., Galhardoni, R. et al. (2015). Neuropathic pain after brachial plexus avulsion - central and peripheral mechanisms. BMC Neurology, 15 (1). https://doi.org/10.1186/s12883-015-0329-x
- Cruccu, G., Truini, A. (2017). A review of Neuropathic Pain: From Guidelines to Clinical Practice. Pain and Therapy, 6 (S1), 35–42. https://doi.org/10.1007/s40122-017-0087-0
- Finnerup, N. B., Attal, N., Haroutounian, S., McNicol, E., Baron, R., Dworkin, R. H. et al. (2015). Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. The Lancet Neurology, 14 (2), 162–173. https://doi.org/10.1016/s1474-4422(14)70251-0
- Moulin, D., Boulanger, A., Clark, A., Clarke, H., Dao, T., Finley, G. et al. (2014). Pharmacological Management of Chronic Neuropathic Pain: Revised Consensus Statement from the Canadian Pain Society. Pain Research and Management, 19 (6), 328–335. https://doi.org/10.1155/2014/754693
- Karra, R., Holten-Rossing, S., Mohammed, D., Parmeggiani, L., Heine, M., Namnún, O. C. (2021). Unmet needs in the management of functional impairment in patients with chronic pain: a multinational survey. Pain Management, 11 (3), 303–314. https://doi.org/10.2217/pmt-2020-0098
- Classification of Chronic Pain (Revised) (2012). IASP Task Force. IASP Taxonomy. Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Available at: https://www.iasp pain.org/PublicationsNews/Content.aspx?ItemNumber=1673 Last accessed: 10.11.2018
- Willis, W. D., Coggeshall, R. E. (1978). Sensor mechanisms of the spinal cord. New York – London: Plenum Press. https://doi.org/10.1007/978-1-4757-1688-7
- Simon, N. G., Franz, C. K., Gupta, N., Alden, T., Kliot, M. (2016). Central Adaptation following Brachial Plexus Injury. World Neurosurgery, 85, 325–332. https://doi.org/10.1016/j.wneu.2015.09.027
- Nickel, F. T., Seifert, F., Lanz, S., Maihöfner, C. (2012). Mechanisms of neuropathic pain. European Neuropsychopharmacology, 22 (2), 81–91. https://doi.org/10.1016/j.euroneuro.2011.05.005
- Quintão, N. L. M., Santos, A. R. S., Campos, M. M., Calixto, J. B. (2008). The role of neurotrophic factors in genesis and maintenance of mechanical hypernociception after brachial plexus avulsion in mice. Pain, 136 (1), 125–133. https://doi.org/10.1016/j.pain.2007.06.027
- Socolovsky, M., Malessy, M., Lopez, D., Guedes, F., Flores, L. (2017). Current concepts in plasticity and nerve transfers: relationship between surgical techniques and outcomes. Neurosurgical Focus, 42 (3), E13. https://doi.org/10.3171/2016.12.focus16431
- Woolf, C. J., Mannion, R. J. (1999). Neuropathic pain: aetiology, symptoms, mechanisms, and management. The Lancet, 353 (9168), 1959–1964. https://doi.org/10.1016/s0140-6736(99)01307-0
- Nicholson, B. (2006). Differential diagnosis: nociceptive and neuropathic pain. The American journal of managed care, 12 (9), S256–S262.
- Dworkin, R. H., Backonja, M., Rowbotham, M. C., Allen, R. R., Argoff, C. R., Bennett, G. J. et al. (2003). Advances in Neuropathic Pain. Archives of Neurology, 60 (11), 1524. https://doi.org/10.1001/archneur.60.11.1524
- Cossins, L., Okell, R. W., Cameron, H., Simpson, B., Poole, H. M., Goebel, A. (2012). Treatment of complex regional pain syndrome in adults: A systematic review of randomized controlled trials published from June 2000 to February 2012. European Journal of Pain, 17 (2), 158–173. https://doi.org/10.1002/j.1532-2149.2012.00217.x
- Tran, D. Q. H., Duong, S., Bertini, P., Finlayson, R. J. (2010). Treatment of complex regional pain syndrome: a review of the evidence. Canadian Journal of Anesthesia/Journal Canadien d’anesthésie, 57 (2), 149–166. https://doi.org/10.1007/s12630-009-9237-0
- Bouhassira, D. (2019). Neuropathic pain: Definition, assessment and epidemiology. Revue Neurologique, 175 (1-2), 16–25. https://doi.org/10.1016/j.neurol.2018.09.016
- Education (2022). IASP terminology. International Association for the Study of Pain. Available at: https://www.iasp-pain.org/Education/Content.aspx
- Bouhassira, D., Attal, N. (2019). The multiple challenges of neuropathic pain. Neuroscience letters, 702, 6–10. https://doi.org/10.1016/j.neulet.2018.11.054
- Scholz, J., Finnerup, N. B., Attal, N., Aziz, Q., Baron, R., Bennett, M. I. et al. (2019). The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain, 160 (1), 53–59. https://doi.org/10.1097/j.pain.0000000000001365
- Gray, P. (2008). Acute neuropathic pain: diagnosis and treatment. Current Opinion in Anaesthesiology, 21 (5), 590–595. https://doi.org/10.1097/aco.0b013e32830c900c
- Colloca, L., Ludman, T., Bouhassira, D., Baron, R., Dickenson, A. H., Yarnitsky, D. et al. (2017). Neuropathic pain. Nature Reviews Disease Primers, 3 (1). https://doi.org/10.1038/nrdp.2017.2
- Woolf, C. J. (2004). Dissecting out mechanisms responsible for peripheral neuropathic pain: Implications for diagnosis and therapy. Life Sciences, 74 (21), 2605–2610. https://doi.org/10.1016/j.lfs.2004.01.003
- Sukhotinsky, I., Ben‐Dor, E., Raber, P., Devor, M. (2004). Key role of the dorsal root ganglion in neuropathic tactile hypersensibility. European Journal of Pain, 8 (2), 135–143. https://doi.org/10.1016/s1090-3801(03)00086-7
- Devor, M. (2006). Sodium Channels and Mechanisms of Neuropathic Pain. The Journal of Pain, 7 (1), S3–S12. https://doi.org/10.1016/j.jpain.2005.09.006
- Samii, M., Bear-Henney, S., Lüdemann, W., Tatagiba, M., Blömer, U. (2001). Treatment of Refractory Pain after Brachial Plexus Avulsion with Dorsal Root Entry Zone Lesions. Neurosurgery, 48 (6), 1269–1277. https://doi.org/10.1227/00006123-200106000-00016
- Zheng, Z., Hu, Y., Tao, W., Zhang, X., Li, Y. (2009). Dorsal Root Entry Zone Lesions for Phantom Limb Pain with Brachial Plexus Avulsion: A Study of Pain and Phantom Limb Sensation. Stereotactic and Functional Neurosurgery, 87 (4), 249–255. https://doi.org/10.1159/000225978
- Chivukula, S., Tempel, Z. J., Chen, C.-J., Shin, S. S., Gande, A. V., Moossy, J. J. (2015). Spinal and Nucleus Caudalis Dorsal Root Entry Zone Lesioning for Chronic Pain: Efficacy and Outcomes. World Neurosurgery, 84 (2), 494–504. https://doi.org/10.1016/j.wneu.2015.04.025
- Be Bertelli, J. A., Ghizoni, M. F. (2008). Pain after avulsion injuries and complete palsy of the brachial plexus. Neurosurgery, 62 (5), 1104–1114. https://doi.org/10.1227/01.neu.0000325872.37258.12
- van Dongen, R., Cohen, S. P., van Kleef, M., Mekhail, N., Huygen, F. (2011). 22. Traumatic Plexus Lesion. Pain Practice, 11 (4), 414–420. https://doi.org/10.1111/j.1533-2500.2011.00451.x
- Lundborg, G., Rosén, B. (2007). Hand function after nerve repair. Acta Physiologica, 189 (2), 207–217. https://doi.org/10.1111/j.1748-1716.2006.01653.x
- Mohanty, C. B., Midha, R. (2015). Nerve Section Causes Brain Reaction. World Neurosurgery, 84 (4), 886–888. https://doi.org/10.1016/j.wneu.2015.06.009
- Haanpää, M. L., Backonja, M.-M., Bennett, M. I., Bouhassira, D., Cruccu, G., Hansson, P. T. et al. (2009). Assessment of Neuropathic Pain in Primary Care. The American Journal of Medicine, 122 (10), S13–S21. https://doi.org/10.1016/j.amjmed.2009.04.006
- Yamamoto, T. (2008). Mechanisms of the development of neuropathic pain and its treatment. Japanese Journal of Leprosy, 77 (3), 215–218. https://doi.org/10.5025/hansen.77.215
- Nonsteroidal anti-inflammatory drugs: add an anti-ulcer drug for patients at high risk only. Always limit the dose and duration of treatment with NSAIDs. (2011). Prescrire international, 20(119), 216–219.
- Walk, D., Backonja, M. M.; Fishman, S. M., Ballantyne, J. C., Rathmell, J. P. (Eds.) (2010). Painful neuropathies. Bonica's management of pain. Philadelphia: Lippincott Williams and Wilkins, 303–313.
- Bentley, J. N., Kashlan, O. N., Sagher, O.; Burchiel, K. J. (Ed.) (2015). Stump, phantom and avulsion pain. Surgical Management of Pain. New York: Thieme, 229–237.
- Vannier, J. L., Belkheyar, Z., Oberlin, C., Montravers, P. (2008). Management of neuropathic pain after brachial plexus injury in adult patients: a report of 60 cases. Annales francaises d'anesthesie et de reanimation, 27 (11), 890–895. https://doi.org/10.1016/j.annfar.2008.08.013
- Schlereth, T. (2020). Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology (deutsche Gesellschaft für Neurologie). Neurological Research and Practice, 2 (1). https://doi.org/10.1186/s42466-020-00063-3
- Lovaglio, A., Socolovsky, M., Di Masi, G., Bonilla, G. (2019). Treatment of neuropathic pain after peripheral nerve and brachial plexus traumatic injury. Neurology India, 67 (7), 32–37. https://doi.org/10.4103/0028-3886.250699
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Olga Dubenko, Olena Tovazhnyanska, Kostiantyn Stepanchenko, Olena Zavalna, Vartanush Florikian

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








