Features of clinical manifestations of generalized periodontal diseases in patients with diabetes mellitus type 2
DOI:
https://doi.org/10.15587/2519-4798.2025.344663Keywords:
generalized parodontal diseases, generalized parodontitis, hygienic indices, diabetes mellitus, osteoporosisAbstract
Aim: to establish the features of the configuration of generalized periodontal diseases and their clinical manifestations in the format of basic characteristics of type 2 diabetes mellitus.
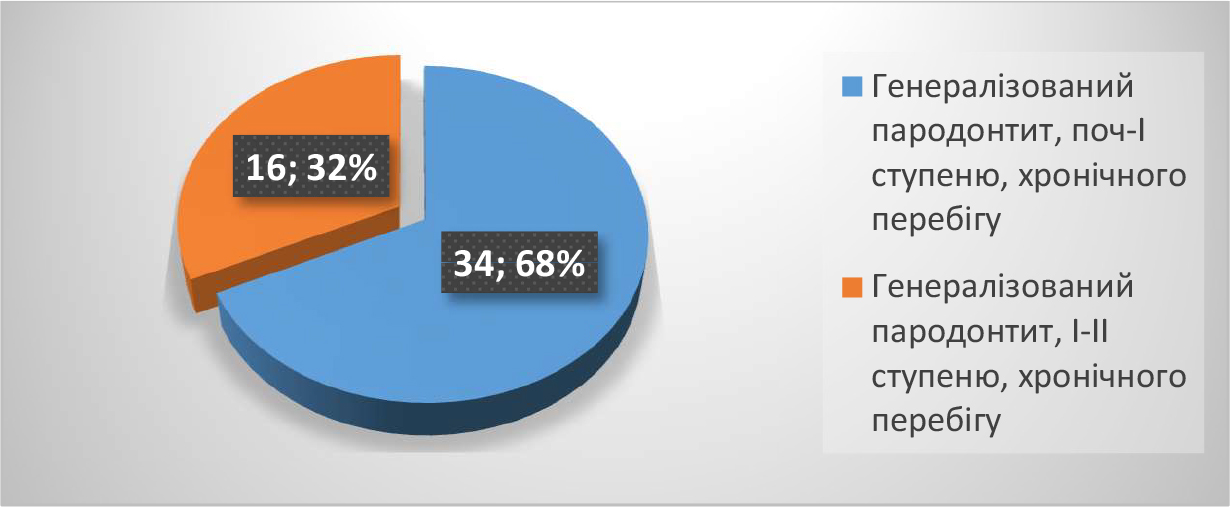
Materials and methods: Clinical, radiological and statistical methods were used. The subjects were 75 patients with type 2 diabetes mellitus, aged 19-44 years (mean age 26±3.8), who made up the main group (M), and 60 patients without signs of diabetes mellitus of a similar age - the comparison group (C). For a detailed analysis of the features of the clinical manifestation of GPD in patients with diabetes mellitus, all patients of the main (M) and comparison (C) groups were divided into several subgroups. M1 subgroup - patients with various forms of gingivitis. M2 subgroup was represented by patients with generalized periodontitis (GP) with type 2 diabetes mellitus as the underlying pathology. The comparative (C) group included two subgroups (C1), (C2) with different forms of gingivitis and periodontal disease, respectively.
Results of our own studies. A high frequency of periodontal disease was diagnosed, reaching 100%, including both independent diseases of the periodontal soft tissues and all components of the periodontal complex, which was characteristic of all age groups and depended on the age of the patients, the duration and stages of type 2 diabetes. Periodontitis was mainly of stages I-II, chronic course prevailed over other stages of periodontal disease (80±4.6%). Radiologically, all patients, regardless of the severity of periodontal disease, had a characteristic vertical and horizontal type of resorption, pronounced osteoporosis of the bone component of the periodontal complex and expansion of the periodontal gap. The advantages and priorities of different segments of periodontal complex damage were traced in no case. For all patients with GP, a high degree of tissue sensitization to bone antigen was finalized, characterizing significant changes in the bone component of the periodontal complex in type 2 diabetes. A hypothesis of a plausible paradigm of the interdependence of GPD and type 2 diabetes as affiliated diseases was proposed as the first stage of further development of this direction.
Conclusions: a direct relationship and interdependence of generalized periodontal diseases in the format of basic characteristics of type 2 diabetes have been established
References
- Khan, M. A. B., Hashim, M. J., King, J. K., Govender, R. D., Mustafa, H., Al Kaabi, J. (2019). Epidemiology of Type 2 Diabetes – Global Burden of Disease and Forecasted Trends. Journal of Epidemiology and Global Health, 10 (1), 107–111. https://doi.org/10.2991/jegh.k.191028.001
- Dye, B. A. (2011). Global periodontal disease epidemiology. Periodontology 2000, 58 (1), 10–25. https://doi.org/10.1111/j.1600-0757.2011.00413.x
- Petersen, P. E., Ogawa, H. (2012). The global burden of periodontal disease: towards integration with chronic disease prevention and control. Periodontology 2000, 60 (1), 15–39. https://doi.org/10.1111/j.1600-0757.2011.00425.x
- Classification and Diagnosis of Diabetes:Standards of Medical Care in Diabetes–2021 (2021). Diabetes Care, 44 (1), S15–S33. https://doi.org/10.2337/dc21-s002
- Kinane, D. F., Stathopoulou, P. G., Papapanou, P. N. (2017). Periodontal diseases. Nature Reviews Disease Primers, 3 (1). https://doi.org/10.1038/nrdp.2017.38
- Zheng, M., Wang, C., Ali, A., Shih, Y. A., Xie, Q., Guo, C. (2021). Prevalence of periodontitis in people clinically diagnosed with diabetes mellitus: a meta-analysis of epidemiologic studies. Acta Diabetologica, 58 (10), 1307–1327. https://doi.org/10.1007/s00592-021-01738-2
- Steele, J. G., Treasure, E. T., O’Sullivan, I., Morris, J., Murray, J. J. (2012). Adult Dental Health Survey 2009: transformations in British oral health 1968–2009. British Dental Journal, 213 (10), 523–527. https://doi.org/10.1038/sj.bdj.2012.1067
- Zachepylo, S. V. (2021). Evaluation of the sensitivity of clinical strains of C. albicans isolated from patients with pharyngomycosis to the combined action of monarda essential oil and antifungal drugs. Bulletin of Problems Biology and Medicine, 1 (159), 184–188. https://doi.org/10.29254/2077-4214-2021-1-159-184-188
- Ananieva, M., Faustova, M., Loban, G., Chumak, Y. (2022). Current approaches of eucast committee to determining susceptibility of odontogenic infections to antibiotics. Actual Problems of the Modern Medicine: Bulletin of Ukrainian Medical Stomatological Academy, 22 (1), 168–174. https://doi.org/10.31718/2077-1096.22.1.168
- Breakpoint tables for interpretation of MICs for antifungal agents (Version 10.0, valid from 2020-02-04) (2020). EUCAST (European Committee on Antimicrobial Susceptibility Testing). Available at: https://www.eucast.org/astoffungi/clinicalbreakpointsforantifungals/
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Anna Lenihevych, Ljudmila Reshetnyk

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








