Characteristics of the structure and composition of the oropharyngeal microbiota in patients with acute tonsillitis depending on smoking status
DOI:
https://doi.org/10.15587/2519-8025.2025.348862Keywords:
tonsillitis, oropharyngeal microbiota, smoking, alpha diversity, beta diversity, dysbiosis, PERMANOVA, SIMPER analysisAbstract
The aim of the study was to compare alpha and beta diversity indices, assess the overall structure and identify taxa of the oropharyngeal microbiota in patients with acute tonsillitis under the influence of smoking.
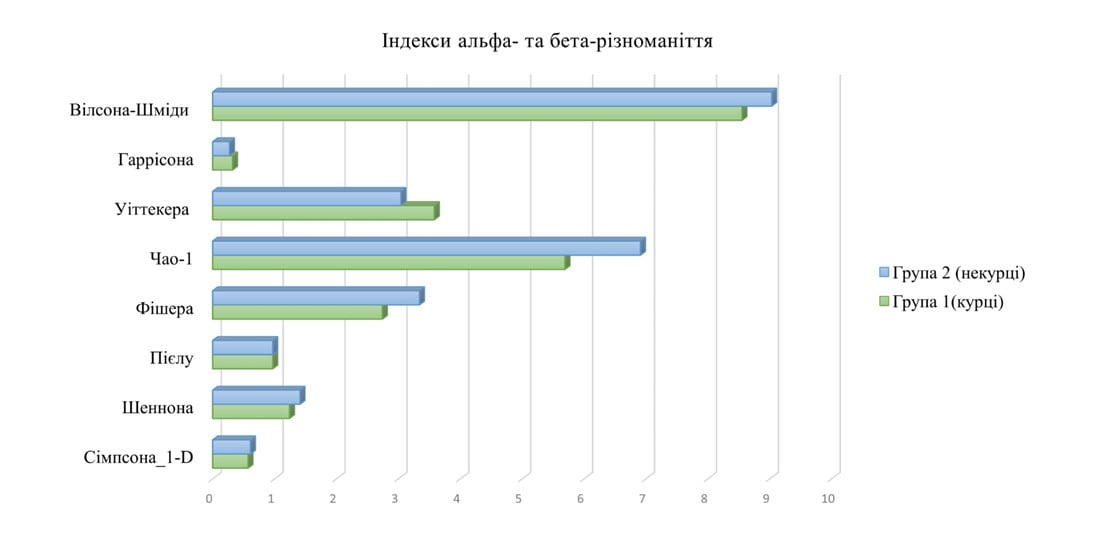
Materials and methods. 54 samples of oropharyngeal swabs from patients with acute tonsillitis were analyzed, which were divided into groups, namely Group 1 (26 people), who smoked, and Group 2 (28 people), who did not smoke. To assess alpha diversity, the Shannon, Simpson, Pielu, Fisher and Chao-1 indices were used, for beta diversity, the Whittaker, Harrison, Wilson-Schmidt and Bray-Curtis indices. The PAST v.4.03 program was used with PERMANOVA, ANOSIM (9999 permutations) and SIMPER statistical analysis.
Results. Analysis of the results of alpha-diversity indices did not reveal statistically significant differences between groups (p > 0.05). The results of beta-diversity indices demonstrated a greater diversity of microbial communities in group 1 (smokers) (Whittaker indices 3.59 vs. 3.05; Harrison indices 0.33 vs. 0.28). The results of multivariate analyses (PERMANOVA, ANOSIM) did not reveal statistically significant differences in the structure of the microbiome of patients with tonsillitis (p > 0.05). SIMPER analysis demonstrated that α-hemolytic streptococci (20.28%), Neisseria spp. (19.59%) belong to taxa responsible for 74.58% of the total intergroup differentiation of the oropharynx, however, they show different colonization densities (5.15 in smokers vs. 4.96 in non-smokers for α-hemolytic Streptococcus spp. and 1.50 in smokers vs. 2.21 in non-smokers for Neisseria spp.)
Conclusion. Regardless of smoking status, the oropharyngeal microbiota of patients with acute tonsillitis is characterized by taxa similarity. However, in patients who smoke, increased variability of microbial communities is observed, in particular, a decrease in commensal bacteria of the genus Corynebacterium spp., a tendency to increase β-hemolytic streptococci and the appearance of fungi of the genus Candida spp., which may affect the course of the inflammatory process
References
- Ashurst, J. V., Weiss, E., Tristram, D., Edgerley-Gibb, L. (2025). Streptococcal pharyngitis. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK525997/
- Nguyen, V. T. N., Ngo, L., Stratton, E., Arriola, D. (2025). Tonsillitis. Primary Care: Clinics in Office Practice, 52 (1), 27–35. https://doi.org/10.1016/j.pop.2024.09.005
- Smith, K. L., Hughes, R., Myrex, P. (2023). Tonsillitis and tonsilloliths: diagnosis and management. American Family Physician, 107 (1), 35–41.
- Bach, L., Ram, A., Ijaz, U. Z., Evans, T. J., Haydon, D. T., Lindström, J. (2023). The Effects of Smoking on Human Pharynx Microbiota Composition and Stability. Microbiology Spectrum, 11 (2). https://doi.org/10.1128/spectrum.02166-21
- Huang, C., Shi, G. (2019). Smoking and microbiome in oral, airway, gut and some systemic diseases. Journal of Translational Medicine, 17 (1). https://doi.org/10.1186/s12967-019-1971-7
- Giordano-Kelhoffer, B., Lorca, C., March Llanes, J., Rábano, A., del Ser, T., Serra, A., Gallart-Palau, X. (2022). Oral Microbiota, Its Equilibrium and Implications in the Pathophysiology of Human Diseases: A Systematic Review. Biomedicines, 10 (8), 1803. https://doi.org/10.3390/biomedicines10081803
- Liu, Y., Qv, W., Ma, Y., Zhang, Y., Ding, C., Chu, M., Chen, F. (2022). The interplay between oral microbes and immune responses. Frontiers in Microbiology, 13. https://doi.org/10.3389/fmicb.2022.1009018
- Rajasekaran, J. J., Krishnamurthy, H. K., Bosco, J., Jayaraman, V., Krishna, K., Wang, T., Bei, K. (2024). Oral Microbiome: A Review of Its Impact on Oral and Systemic Health. Microorganisms, 12 (9), 1797. https://doi.org/10.3390/microorganisms12091797
- Wüthrich, T., de Brot, S., Richina, V., Mostacci, N., Baumann, Z., Leborgne, N. G. F. et al. (2024). Cigarette smoke-induced disordered microbiota aggravates the severity of influenza A virus infection. MSystems, 9 (12). https://doi.org/10.1128/msystems.00790-24
- Hattan, A. A., Hattan, E. A., Alqahtani, A. M., Alqutaym, O. S., Alqahtani, R. O., Alzahrani, K. G. et al. (2018). Impact of tobacco smoking on oral microbiota – a case-control study. Medical Perspectives, 23 (3), 13–20. https://doi.org/10.26641/2307-0404.2018.3.147948
- Kumar, P. S., Matthews, C. R., Joshi, V., de Jager, M., Aspiras, M. (2011). Tobacco Smoking Affects Bacterial Acquisition and Colonization in Oral Biofilms. Infection and Immunity, 79 (11), 4730–4738. https://doi.org/10.1128/iai.05371-11
- Joshi, V., Matthews, C., Aspiras, M., de Jager, M., Ward, M., Kumar, P. (2014). Smoking decreases structural and functional resilience in the subgingival ecosystem. Journal of Clinical Periodontology, 41 (11), 1037–1047. https://doi.org/10.1111/jcpe.12300
- Tonzylit. Unifikovanyi klinichnyi protokol pervynnoi, vtorynnoi (spetsializovanoi) ta tretynnoi (vysokospetsializovanoi) medychnoi dopomohy (2021). Ministerstvo okhorony zdorovia Ukrainy. Available at: https://www.dec.gov.ua/wp-content/uploads/2021/04/2021_639_ykpmd_tonzylit_dd.pdf
- Minukhin, V. V., Kovalenko, N. I., Zamazii, T. M. (2014). Modul 3. Chastyna 3. Umovno-patohenni mikroorhanizmy. Kharkiv: KhNMU.
- Goodfellow, M., Kämpfer, P., Busse, H. J., Trujillo, M. E., Suzuki, K. I., Ludwig, W. et al. (Eds.) (2012). Bergey's Manual of Systematic Bacteriology: Volume 5: The Actinobacteria. New York: Springer-Verlag.
- Klymniuk, S. I., Sytnyk, I. O., Shyrobokov, V. P. (2018). Praktychna mikrobiolohiia. Vinnytsia: Nova Knyha.
- Leontiev, D. V. (2007). Florystychnyi analiz v mikolohii. Kharkiv: Vydavnycha hrupa «Osnova», 160.
- WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human participants. World Medical Association (2024). Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Pro zatverdzhennia Poriadku provedennia klinichnykh vyprobuvan likarskykh zasobiv ta ekspertyzy materialiv klinichnykh vyprobuvan i Typovoho polozhennia pro komisii z pytan etyky: Nakaz Ministerstva okhorony zdorovia Ukrainy No. 690. 23.09.2009. Available at: https://zakon.rada.gov.ua/laws/show/z1010-09#Text
- Wu, J., Peters, B. A., Dominianni, C., Zhang, Y., Pei, Z., Yang, L. Et al. (2016). Cigarette smoking and the oral microbiome in a large study of American adults. The ISME Journal, 10 (10), 2435–2446. https://doi.org/10.1038/ismej.2016.37
- Mohammed, L. I., Razali, R., Zakaria, Z. Z., Benslimane, F. M., Cyprian, F., Al-Asmakh, M. (2024). Smoking induced salivary microbiome dysbiosis and is correlated with lipid biomarkers. BMC Oral Health, 24 (1). https://doi.org/10.1186/s12903-024-04340-4
- Moon, J.-H., Lee, J.-H. (2016). Probing the diversity of healthy oral microbiome with bioinformatics approaches. BMB Reports, 49 (12), 662–670. https://doi.org/10.5483/bmbrep.2016.49.12.164
- Chattopadhyay, S., Malayil, L., Chopyk, J., Smyth, E., Kulkarni, P., Raspanti, G. et al. (2024). Oral microbiome dysbiosis among cigarette smokers and smokeless tobacco users compared to non-users. Scientific Reports, 14 (1). https://doi.org/10.1038/s41598-024-60730-2
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Nataliia Kravets

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.







