Clinical efficacy of the symbiotic drug Lotardi-A in the complex therapy of patients with irritable bowel syndrome in metabolic-associated fatty liver disease
DOI:
https://doi.org/10.15587/2519-4798.2025.329828Keywords:
non-alcoholic fatty liver disease/metabolically associated fatty liver disease, irritable bowel syndrome, obesity, metabolic disorders, microbiome, diagnosis, treatment (probiotics)Abstract
Irritable bowel syndrome (IBS) and metabolite-associated fatty liver disease (MAFLD) are among the most common gastrointestinal and liver diseases encountered in primary and secondary care.
The aim of the study was to determine the clinical efficacy of treatment with the symbiotic drug Lotardi-A in the complex therapy of patients with IBS with MAFLD.
Materials and methods. The study included 60 patients with IBS with MAFLD. Patients with IBS in combination with MAFLD were divided into two groups, depending on the method of treatment. The first group of patients (group I - n= 30) received only basic therapy aimed at correcting the functional state of the intestine and liver. The second group of patients (group II - n= 30), in addition to the basic treatment, received the symbiotic drug Lothardi-A.
Results of the study. Additional administration of the symbiotic Lotardi-A to the subjects contributed to positive changes in the quantitative and qualitative composition of the colon microflora. A significant increase in the number of Bifidobacterium, Lactobacillus was determined. Evaluation of the dynamics of biochemical blood parameters after treatment, indicating the functional state of the liver in patients with IBS with MAFLD confirms more pronounced positive changes in laboratory parameters of cholestatic syndrome in the second group of patients. A significant decrease in the signs of cytolytic syndrome was also found.
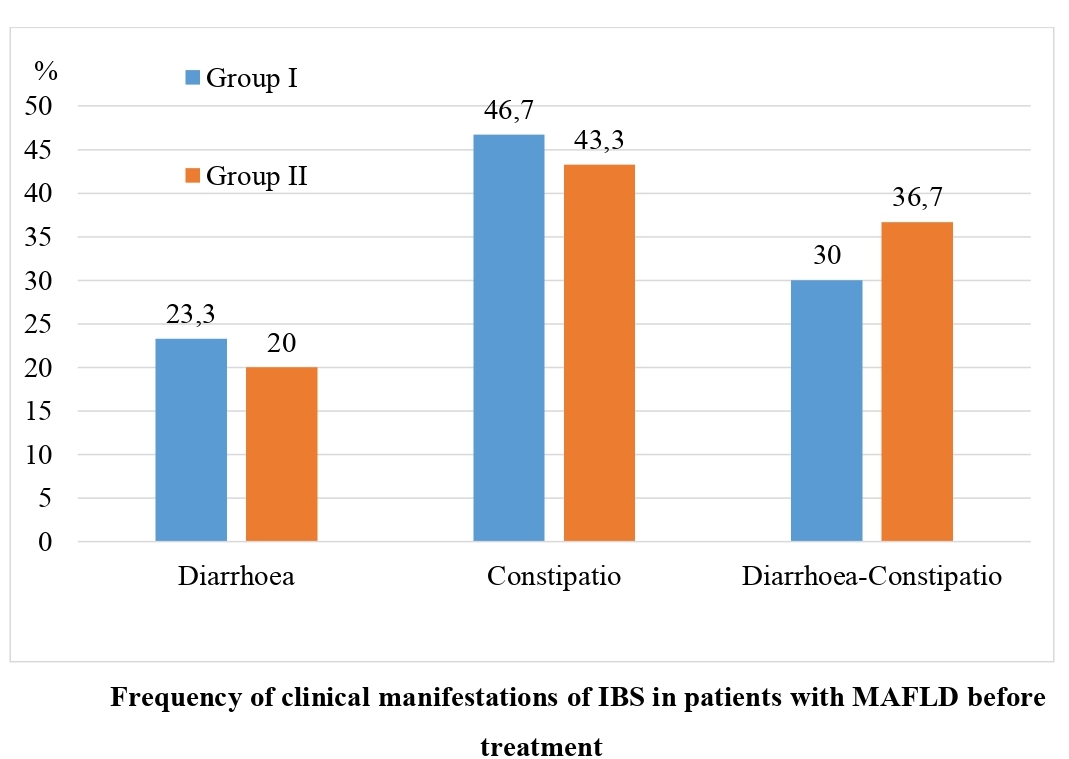
Conclusions: In patients with IBS and MAFLD, it is clinically more often manifested by constipation, namely in 43.3-46.7 %, respectively. These changes occur against the background of colon dysbiosis, mainly of the II and I stages (in 50.0 % and 36.7-40.0 % of the subjects). The treatment of patients with IBS and MAFLD should be comprehensive and include probiotic drugs. Prescription of Lothardi-A is an effective method for the correction of clinical manifestations of IBS, and is also a necessary component for the treatment of MAFLD and correction of dysbiotic changes. At the same time, in patients of group I with MAFLD and IBS with constipation, an increase in the frequency of defecation by 30.0 % (p<0.01) was found, while in patients of group I - only by 10.0 % (p<0.05). In 26.7 % of patients in group II after complex treatment, dysbiosis was not detected during repeated examination, while in group I, we did not find such patients. The additional administration of a symbiotic complex to patients with IBS in MAFLD is an effective means of complex treatment to reduce the severity of disorders of the functional state of the liver and lipid metabolism. At the same time, in patients of group II, a more pronounced significant decrease in serum ALT activity was found (decrease by 43.63±0.37 U/l - p<0.01). The same trend was found when assessing the level of triglycerides in the blood serum (decrease by 1.65±0.03 mmol/l - p<0.01)
References
- Purssell, H., Whorwell, P. J., Athwal, V. S., Vasant, D. H. (2021). Non-alcoholic fatty liver disease in irritable bowel syndrome: More than a coincidence? World Journal of Hepatology, 13 (12), 1816–1827. https://doi.org/10.4254/wjh.v13.i12.1816
- Oka, P., Parr, H., Barberio, B., Black, C. J., Savarino, E. V., Ford, A. C. (2020). Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology, 5 (10), 908–917. https://doi.org/10.1016/s2468-1253(20)30217-x
- Sperber, A. D., Dumitrascu, D., Fukudo, S., Gerson, C., Ghoshal, U. C., Gwee, K. A. et al. (2016). The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut, 66 (6), 1075–1082. https://doi.org/10.1136/gutjnl-2015-311240
- Black, C. J., Ford, A. C. (2020). Global burden of irritable bowel syndrome: trends, predictions and risk factors. Nature Reviews Gastroenterology & Hepatology, 17 (8), 473–486. https://doi.org/10.1038/s41575-020-0286-8
- Targher, G., Byrne, C. D., Tilg, H. (2020). NAFLD and increased risk of cardiovascular disease: clinical associations, pathophysiological mechanisms and pharmacological implications. Gut, 69 (9), 1691–1705. https://doi.org/10.1136/gutjnl-2020-320622
- Cotter, T. G., Charlton, M. (2019). Nonalcoholic Steatohepatitis After Liver Transplantation. Liver Transplantation, 26 (1), 141–159. https://doi.org/10.1002/lt.25657
- Haldar, D., Kern, B., Hodson, J., Armstrong, M. J., Adam, R., Berlakovich, G. et al. (2019). Outcomes of liver transplantation for non-alcoholic steatohepatitis: A European Liver Transplant Registry study. Journal of Hepatology, 71 (2), 313–322. https://doi.org/10.1016/j.jhep.2019.04.011
- Holtmann, G. J., Ford, A. C., Talley, N. J. (2016). Pathophysiology of irritable bowel syndrome. The Lancet Gastroenterology & Hepatology, 1 (2), 133–146. https://doi.org/10.1016/s2468-1253(16)30023-1
- Khalil, Md. M., Munira, S., Alam, Md. M., Appolo, A. M., Sayeed, M. Md. A., Islam, A. et al. (2024). Prevalence of Nonalcoholic Fatty Liver Disease [NAFLD] and Metabolic dysfunction associated Fatty Liver Disease [MAFLD] in patients with Irritable Bowel Syndrome [IBS]. SN Comprehensive Clinical Medicine, 6 (1). https://doi.org/10.1007/s42399-024-01675-5
- Zeng, F., Su, X., Liang, X., Liao, M., Zhong, H., Xu, J. et al. (2024). Gut microbiome features and metabolites in non-alcoholic fatty liver disease among community-dwelling middle-aged and older adults. BMC Medicine, 22 (1). https://doi.org/10.1186/s12916-024-03317-y
- Safari, Z., Gérard, P. (2019). The links between the gut microbiome and non-alcoholic fatty liver disease (NAFLD). Cellular and Molecular Life Sciences, 76 (8), 1541–1558. https://doi.org/10.1007/s00018-019-03011-w
- Kolodziejczyk, A. A., Zheng, D., Shibolet, O., Elinav, E. (2019). The role of the microbiome in NAFLD and NASH. EMBO Molecular Medicine, 11 (2). https://doi.org/10.15252/emmm.201809302
- Canfora, E. E., Meex, R. C. R., Venema, K., Blaak, E. E. (2019). Gut microbial metabolites in obesity, NAFLD and T2DM. Nature Reviews Endocrinology, 15(5), 261–273. https://doi.org/10.1038/s41574-019-0156-z
- Chen, J., Vitetta, L. (2020). Gut Microbiota Metabolites in NAFLD Pathogenesis and Therapeutic Implications. International Journal of Molecular Sciences, 21 (15), 5214. https://doi.org/10.3390/ijms21155214
- Jiao, N., Baker, S. S., Chapa-Rodriguez, A., Liu, W., Nugent, C. A., Tsompana, M. et al. (2017). Suppressed hepatic bile acid signalling despite elevated production of primary and secondary bile acids in NAFLD. Gut, 67 (10), 1881–1891. https://doi.org/10.1136/gutjnl-2017-314307
- Brody, H. (2020). The gut microbiome. Nature, 577 (7792), S5–S5. https://doi.org/10.1038/d41586-020-00194-2
- Si, J., Lee, G., You, H. J., Joo, S. K., Lee, D. H., Ku, B. J. et al. (2021). Gut microbiome signatures distinguish type 2 diabetes mellitus from non-alcoholic fatty liver disease. Computational and Structural Biotechnology Journal, 19, 5920–5930. https://doi.org/10.1016/j.csbj.2021.10.032
- Iino, C., Endo, T., Mikami, K., Hasegawa, T., Kimura, M., Sawada, N. et al. (2019). Significant decrease in Faecalibacterium among gut microbiota in nonalcoholic fatty liver disease: a large BMI- and sex-matched population study. Hepatology International, 13 (6), 748–756. https://doi.org/10.1007/s12072-019-09987-8
- Lee, G., You, H. J., Bajaj, J. S., Joo, S. K., Yu, J., Park, S. et al. (2020). Distinct signatures of gut microbiome and metabolites associated with significant fibrosis in non-obese NAFLD. Nature Communications, 11 (1). https://doi.org/10.1038/s41467-020-18754-5
- Su, X., Chen, S., Liu, J., Feng, Y., Han, E., Hao, X. et al. (2023). Composition of gut microbiota and non‐alcoholic fatty liver disease: A systematic review and meta‐analysis. Obesity Reviews, 25 (1). https://doi.org/10.1111/obr.13646
- Cammarota, G., Ianiro, G., Ahern, A., Carbone, C., Temko, A., Claesson, M. J. et al. (2020). Gut microbiome, big data and machine learning to promote precision medicine for cancer. Nature Reviews Gastroenterology & Hepatology, 17 (10), 635–648. https://doi.org/10.1038/s41575-020-0327-3
- Chong, P. P., Chin, V. K., Looi, C. Y., Wong, W. F., Madhavan, P., Yong, V. C. (2019). The Microbiome and Irritable Bowel Syndrome – A Review on the Pathophysiology, Current Research and Future Therapy. Frontiers in Microbiology, 10. https://doi.org/10.3389/fmicb.2019.01136
- Enck, P., Aziz, Q., Barbara, G., Farmer, A. D., Fukudo, S., Mayer, E. A. et al. (2016). Irritable bowel syndrome. Nature Reviews Disease Primers, 2 (1). https://doi.org/10.1038/nrdp.2016.14
- Menees, S., Chey, W. (2018). The gut microbiome and irritable bowel syndrome. F1000Research, 7, 1029. https://doi.org/10.12688/f1000research.14592.1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Yelyzaveta Sirchak

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








