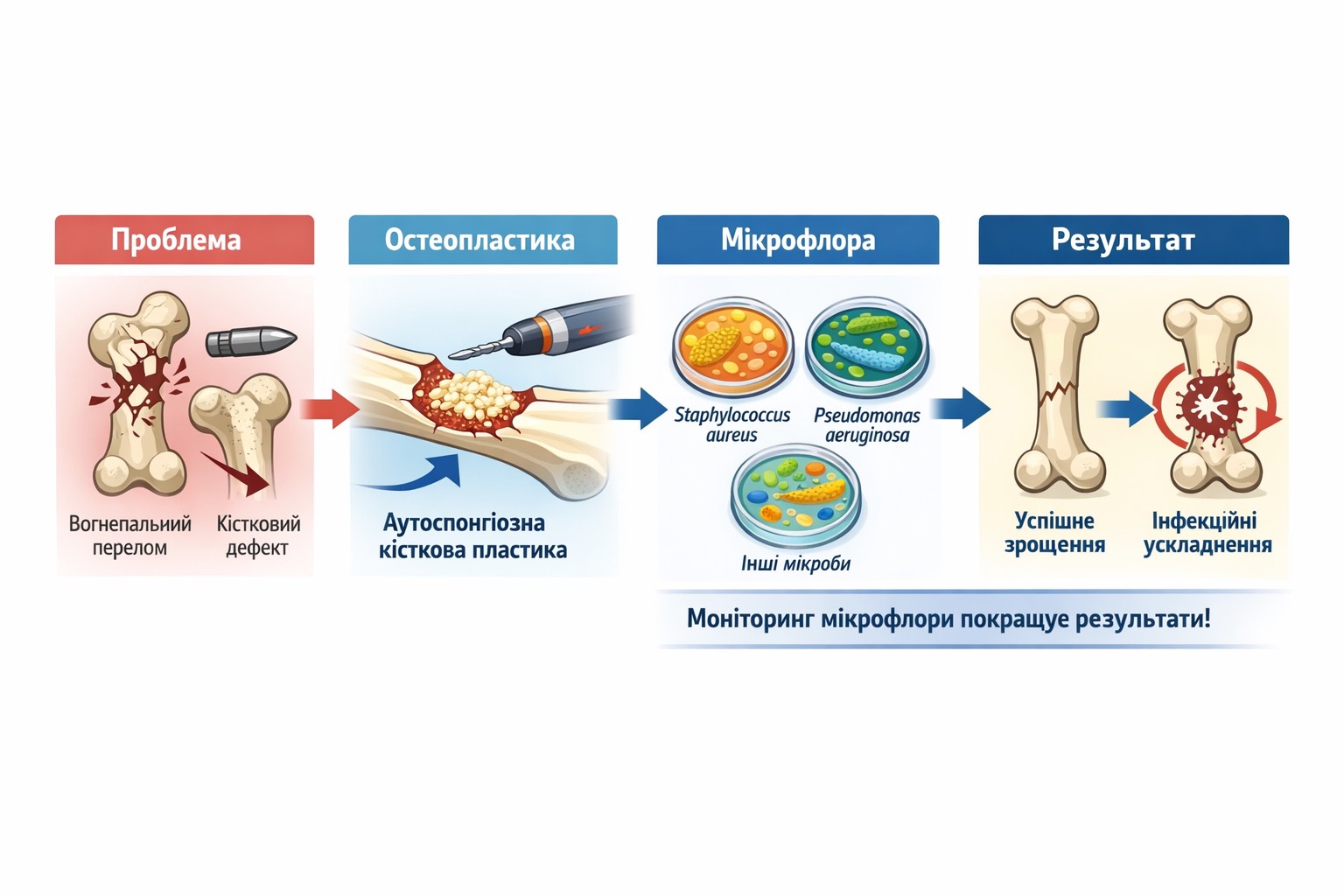
Microbiological predictors of clinical outcomes of autospongious osteoplasty in patients with gunshot fractures and bone tissue defects
DOI:
https://doi.org/10.15587/2519-4798.2025.348416Keywords:
combat trauma, gunshot fractures, bone defects, osteoplasty, bone repairAbstract
The effectiveness of bone grafting depends not only on the size of the defect or the type of osteoplastic material used, but also on the microbial spectrum of the wound, the level of bacterial load, and the presence of biofilm.
Objective. To assess the condition of wound microbiocenosis in gunshot fractures of long bones with bone tissue defects and its role in predicting the clinical outcome of autospongious osteoplasty.
Materials and Methods. This study analyzed the results of bacteriological examination of wound contents and clinical indicators of autospongious osteoplasty in 40 patients with gunshot fractures of long bones accompanied by bone tissue defects. Clinical outcomes were assessed using the modified Neer–Grantham–Shelton 100-point scale. Bacteriological testing was performed according to standard protocols. Statistical analysis was conducted using IBM SPSS Statistics 27.0.1, with a significance level set at p≤0.05.
Results. Excellent outcomes of autospongious osteoplasty were observed in 4 (10.0 %) patients, good in 11 (27.5 %), satisfactory in 17 (42.5 %), and poor in 8 (20.0 %). The analysis of the microbial species composition revealed significantly worse outcomes in cases of wound contamination with gram-negative flora (τ=–0.32, p=0.004), particularly members of the Enterobacteriaceae family (τ=–0.26, p=0.02), including Klebsiella pneumoniae (τ=–0.22, p=0.04), ESKAPE group pathogens (τ=-0,35, р=0,002). Conversely, identification of Bacillus species was associated with significantly higher odds of achieving excellent clinical outcomes (OR=51.00, CI (3.22-808.36), p=0.001).
Conclusion. Monitoring the state of the wound microbiocenosis in patients with gunshot fractures and bone tissue defects is of both diagnostic and prognostic value in determining the clinical success of autologous bone grafting
References
- Hrytsai, M., Kolov, H., Sabadosh, V., Vyderko, R., Polovyi, A., Нutsailiuk, V. (2024). Main Surgical Methods of Critical Tibial Bone Defects Replacement (Literature Review). Part II. Terra Orthopaedica, 2 (121), 45–53. https://doi.org/10.37647/2786-7595-2024-121-2-45-53
- Rodionov А., Nosivets, D., Bets, V., Voronets, V., Denysiuk, M. (2024). Surgical Treatment of Bone Defects of the Extremities after Gunshot Injuries. Orthopaedics Traumatology and Prosthetics, 4, 76–81. https://doi.org/10.15674/0030-59872024476-81
- Korol, S. (2021). Bone grafting in the system of specialized treatment of victims with battle limb injuries. Trauma, 19 (1), 20–26. https://doi.org/10.22141/1608-1706.1.19.2018.126659
- Burianov, O., Kvasha, V., Sobolevskiy, Y., Yarmoliuk, Y., Klapchuk, Y., Los, D. et al. (2024). Methodological principles of diagnosis verification and treatment tactics determination in combat limb injuries with bone defects. Orthopaedics Traumatology and Prosthetics, 4, 5–13. https://doi.org/10.15674/0030-5987202345-13
- Hrytsai, M., Kolov, H., Sabadosh, V., Vyderko, R., Polovyi, A., Нutsailiuk, V. (2024). Main Surgical Methods of Critical Tibial Bone Defects Replacement (Literature Review): Part I. Terra Orthopaedica, 1 (120), 42–49. https://doi.org/10.37647/2786-7595-2024-120-1-42-49
- Krishtafor, D. A., Krishtafor, A. A., Halushchak, A. Y., Mynka, V. Y., Seleznova, U. V., Grabova, G. Y. (2023). Antibacterial therapy for combat gunshot trauma: eight years after (retrospective observational study). Emergency Medicine, 19 (4), 241–248. https://doi.org/10.22141/2224-0586.19.4.2023.1591
- Rudenko, M., Dakal, A. (2023). Pathophysiology of flammable injuries of main vessels: analysis of modern research. Modern Medicine, Pharmacy and Psychological Health, 2, 18–22. https://doi.org/10.32689/2663-0672-2023-2-3
- Fomin, O. O., Kovalchuk, V. P., Fomina, N. S., Zheliba, M. D., Dobrovanov, O., Kralynskyi, K. (2019). Treatment of purulent-inflammatory complications in a combat gunshot trauma. Suchasni medychni tekhnolohii, 2, 34–39.
- Hrytsai, M. P., Poliachenko, Yu. V., Tsokalo, V. M., Kolov, H. B., Yevlantieva, T. A. (2023). Treatment Tactics in Case of Infectious Complications in Patients with Combat Injuries of the Musculoskeletal System (according to the Clinic’s Own Experience). Terra Orthopaedica, 1 (116), 46–57. https://doi.org/10.37647/2786-7595-2023-116-1-46-57
- Fomin, O. O., Fomina, N. S., Lazarenko, Yu. V., Shalyhin, S. M., Shamin, A. M., Kuziv, Ye. L., Martsynkovskyi, I. P. (2020). Features of the use of antibiotics in the treatment of gunshot fractures of long bones. Current Aspects of Military Medicine. Suchasni Aspekty Viiskovoi Medytsyny, 27 (2), 194–200. https://doi.org/10.32751/2310-4910-2020-27-42
- Melnyk, O., Vorobets, D., Chaplyk, V., Vorobets, M., Fafula, R., Besedina, A., Vorobets, Z. (2025). Profile of antibiotic resistance of the main infectious contaminants on the wound surface of wounded men in the Russian-Ukrainian war. Wiadomości Lekarskie, 2, 295–302. https://doi.org/10.36740/wlek/197142
- Bieler, D., Kollig, E., Weber, W., Hackenberg, L., Pavlu, F., Franke, A., Friemert, B., Achatz, G. (2024). Microbiological challenges in the treatment of war injuries. Die Unfallchirurgie, 127 (7), 509–514. https://doi.org/10.1007/s00113-024-01444-y
- Pallett, S. J. C., Trompeter, A., Basarab, M., Moore, L. S. P., Boyd, S. E. (2023). Multidrug-resistant infections in war victims in Ukraine. The Lancet Infectious Diseases, 23 (8), e270–e271. https://doi.org/10.1016/s1473-3099(23)00391-2
- Ljungquist, O., Nazarchuk, O., Kahlmeter, G., Andrews, V., Koithan, T., Wasserstrom, L. et al. (2023). Highly multidrug-resistant Gram-negative bacterial infections in war victims in Ukraine, 2022. The Lancet Infectious Diseases, 23 (7), 784–786. https://doi.org/10.1016/s1473-3099(23)00291-8
- Neer, C. S. (1970). Displaced Proximal Humeral Fractures. Part I. Classification and Evaluation. The Journal of Bone & Joint Surgery, 52 (6), 1077–1089. https://doi.org/10.2106/00004623-197052060-00001
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates, 567.
- Pipitò, L., Rubino, R., D’Agati, G., Bono, E., Mazzola, C. V., Urso, S. et al. (2025). Antimicrobial Resistance in ESKAPE Pathogens: A Retrospective Epidemiological Study at the University Hospital of Palermo, Italy. Antibiotics, 14 (2), 186. https://doi.org/10.3390/antibiotics14020186
- Sathe, N., Beech, P., Croft, L., Suphioglu, C., Kapat, A., Athan, E. (2023). Pseudomonas aeruginosa: Infections and novel approaches to treatment “Knowing the enemy” the threat of Pseudomonas aeruginosa and exploring novel approaches to treatment. Infectious Medicine, 2 (3), 178–194. https://doi.org/10.1016/j.imj.2023.05.003
- Steinhausen, E., Lefering, R., Glombitza, M., Brinkmann, N., Vogel, C., Mester, B., Dudda, M. (2021). Bioactive glass S53P4 vs. autologous bone graft for filling defects in patients with chronic osteomyelitis and infected non-unions – a single center experience. Journal of Bone and Joint Infection, 6 (4), 73–83. https://doi.org/10.5194/jbji-6-73-2021
- Giannitsioti, E., Salles, M. J., Mavrogenis, A., Rodriguez-Pardo, D., Los-Arcos, I., Ribera, A. et al. (2022). Osteosynthesis-associated infection of the lower limbs by multidrug-resistant and extensively drug-resistant Gram-negative bacteria: a multicentre cohort study. Journal of Bone and Joint Infection, 7 (6), 279–288. https://doi.org/10.5194/jbji-7-279-2022
- De Prisco, M., Manente, R., Santella, B., Serretiello, E., Dell’Annunziata, F., Santoro, E. et al. (2024). Impact of ESKAPE Pathogens on Bacteremia: A Three-Year Surveillance Study at a Major Hospital in Southern Italy. Antibiotics, 13 (9), 901. https://doi.org/10.3390/antibiotics13090901
- Shen, J., Wei, Z., Wang, S., Wang, X., Lin, W., Liu, L., Wang, G. (2023). Treatment of infected bone defects with the induced membrane technique. Bone & Joint Research, 12 (9), 546–558. https://doi.org/10.1302/2046-3758.129.bjr-2022-0439.r2
- Song, M., Sun, J., Lv, K., Li, J., Shi, J., Xu, Y. (2025). A comprehensive review of pathology and treatment of staphylococcus aureus osteomyelitis. Clinical and Experimental Medicine, 25 (1). https://doi.org/10.1007/s10238-025-01595-1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Oleksandr Lytvyniuk, Volodymyr Fishchenko

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








