Evaluation of the impact of chronic wound treatment on the quality of life of patients in Ukraine based on the Wound-QoL-17 questionnaire
DOI:
https://doi.org/10.15587/2519-4798.2025.348430Keywords:
chronic wounds, health-related quality of life, HRQoL, Wound-QoL-17, patient-centered care, rehabilitation, clinical effectiveness, social integrationAbstract
Chronic wounds represent a significant medical and social problem, substantially reducing patients’ health-related quality of life (HRQoL) across physical, emotional, functional, and social domains. Standardized questionnaires, particularly the Wound-QoL-17, are widely used internationally to assess HRQoL; however, studies in Ukraine remain scarce.
Aim. To evaluate the impact of treatment based on the developed methodology for chronic wounds on patients’ HRQoL by assessing physical discomfort, emotional state, functional limitations, and socio-economic burden using the Wound-QoL-17 questionnaire.
Materials and Methods. The study was conducted at the Burn Unit of the Municipal Non-Profit Enterprise “Medical Center of Kyiv City”. Patients with chronic wounds completed the Wound-QoL-17 questionnaire twice – at baseline and after wound healing. The questionnaire included 17 items covering key aspects of patients’ lives.
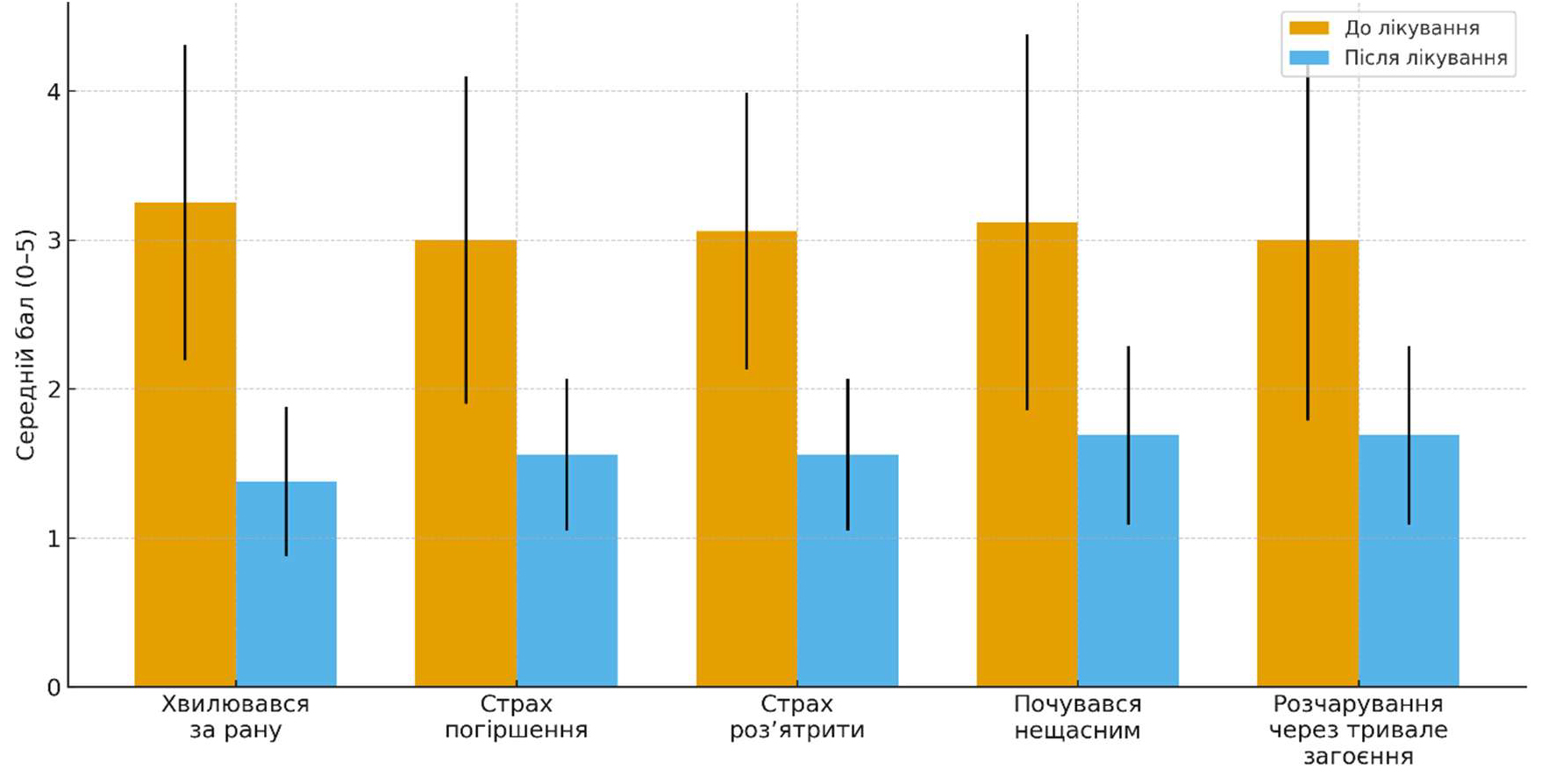
Results. All 17 items showed statistically significant improvements (p < 0.001). The most pronounced effects were observed in pain reduction (3.25 ± 0.93 before vs. 1.56 ± 0.73 after treatment; d = 1.78), decreased dependence on others (3.12 ± 1.02 vs. 1.44 ± 0.51; d = 1.93), and reduced financial burden (for the healthcare system) (3.31 ± 1.14 vs. 1.62 ± 0.62; d = 1.57). Emotional well-being and functional activity also improved significantly, including mobility, stair climbing, and performance of daily activities.
Conclusions. Treatment of chronic wounds leads to a comprehensive improvement in HRQoL, supported by statistically and clinically significant results. The Wound-QoL-17 questionnaire is a valid tool for evaluating treatment effectiveness and may be recommended for integration into Ukrainian healthcare practice
References
- Zhu, X., Olsson, M. M., Bajpai, R., Järbrink, K., Tang, W. E., Car, J. (2021). Health‐related quality of life and chronic wound characteristics among patients with chronic wounds treated in primary care: A cross‐sectional study in Singapore. International Wound Journal, 19 (5), 1121–1132. https://doi.org/10.1111/iwj.13708
- Maheshwari, G. (2024). Chronic wounds: a rising public health concern. Wounds Asia, 7 (1). Available at: https://woundsasia.com/journal-articles/chronic-wounds-a-rising-public-health-concern
- Secco, J., Spinazzola, E., Pittarello, M., Ricci, E., Pareschi, F. (2024). Clinically validated classification of chronic wounds method with memristor-based cellular neural network. Scientific Reports, 14 (1). https://doi.org/10.1038/s41598-024-81521-9
- Price, P., Krasner, D. L.; Krasner, D. L., Rodeheaver, G. T., Sibbald, R. G., Woo, K. Y. (Eds.) (2012). Health-related quality of life and chronic wounds: Evidence and implications for practice. Chronic Wound Care: A Clinical Source Book for Healthcare Professionals. Malvern: HMP Communications.
- Herber, O. R., Schnepp, W., Rieger, M. A. (2007). A systematic review on the impact of leg ulceration on patients’ quality of life. Health and Quality of Life Outcomes, 5. https://doi.org/10.1186/1477-7525-5-44
- Erfurt-Berge, C., Renner, R. (2020). Quality of life in patients with chronic wounds. Hautarzt, 71 (11), 863–869. https://doi.org/10.1007/s00105-020-04673-5
- Hongying, Z., Chunmei, H., Lijuan, C., Miao, T., Jingying, X., Hongmei, J. et al. (2025). The current status and influencing factors of quality of life of chronic wound patients based on Wound-QoL scale: A cross-sectional study. Medicine, 104 (27), e42961. https://doi.org/10.1097/md.0000000000042961
- EuroQol Group. EQ-5D-5L. Available at: https://euroqol.org/
- About the questionnaire. Wound-QoL. Available at: https://www.wound-qol.com/about/
- Blome, C., Baade, K., Sebastian Debus, E., Price, P., Augustin, M. (2014). The “Wound-QoL”: A short questionnaire measuring quality of life in patients with chronic wounds based on three established disease‐specific instruments. Wound Repair and Regeneration, 22 (4), 504–514. https://doi.org/10.1111/wrr.12193
- Janke, T. M., Kozon, V., Valiukeviciene, S., Rackauskaite, L., Reich, A., Stępień, K. et al. (2023). Validation of the Wound‐QoL‐17 and the Wound‐QoL‐14 in a European sample of 305 patients with chronic wounds. International Wound Journal, 21 (3). https://doi.org/10.1111/iwj.14505
- Augustin, M., Conde Montero, E., Zander, N., Baade, K., Herberger, K., Debus, E. S. et al. (2017). Validity and feasibility of the wound‐QoL questionnaire on health‐related quality of life in chronic wounds. Wound Repair and Regeneration, 25 (5), 852–857. https://doi.org/10.1111/wrr.12583
- Markin, A. (2021). Results of studying the sensitivity of Ukrainian version of Haemo-QoL Questionnaire. Child`S Health, 13 (3), 338–344. https://doi.org/10.22141/2224-0551.13.3.2018.132909
- Dührkoop, E., Malihi, L., Erfurt-Berge, C., Heidemann, G., Przysucha, M., Busch, D., Hübner, U. (2024). Automatic Classification of Wound Images Showing Healing Complications: Towards an Optimised Approach for Detecting Maceration. Studies in Health Technology and Informatics, 317, 347–355. https://doi.org/10.3233/shti240877
- Naumenko, L. Yu., Horehliad, O. M. (2018). Quality of Life Assessment for Patients with Negative Pressure Therapy of Ballistic Injuries of the Extremities. Suchasni medychni tekhnolohii, 3, 60–64.
- Litwack, K. (2015). Pain Management in Military Trauma. Critical Care Nursing Clinics of North America, 27 (2), 235–246. https://doi.org/10.1016/j.cnc.2015.02.005
- Trush O. S. (2025). Stresostiikist medychnykh pratsivnykiv u voiennyi chas yak chynnyk zberezhennia psykhichnoho zdorovia. KhV Mizhnarodna Naukovo-Praktychna Konferentsiia, 411.
- Petrenko, O. M. (2017). Analysis of the results of conservative and surgical treatment in patients with chronic wounds by traditional methods. Ukrainskyi medychnyi chasopys, 6, 133–135.
- Fagerdahl, A.-M., Bergstrom, G. (2018). Translation and Validation of a Wound-specific, Quality-of-life Instrument (The Wound-QoL) in a Swedish Population. Ostomy Wound Management, 64 (5), 40–46. https://doi.org/10.25270/owm.2018.5.4046
- Augustin, M., Baade, K., Heyer, K., Price, P. E., Herberger, K., Wild, T. et al. (2017). Quality‐of‐life evaluation in chronic wounds: comparative analysis of three disease‐specific questionnaires. International Wound Journal, 14 (6), 1299–1304. https://doi.org/10.1111/iwj.12803
- Integrating the response to mental health disorders and other chronic diseases in health care systems (2020). Geneva: WHO. Available at: https://www.who.int/publications/i/item/9789241506793
- Schwartz, M. M., Ljosaa, T. M., Pukstad, B. S., Utvær, B. K. (2025). Cardiff Wound Impact Schedule—Validity, Reliability and Dimensionality of the Norwegian Version. International Wound Journal, 22 (6). https://doi.org/10.1111/iwj.70697
- Pokydko, M. I., Balabuieva, V. V., Filippov, S. V., Zarezenko, T. P., Ordatii, A. V., Bohachuk, M. H. (2024). The multidisciplinary approach to the treatment of chronic wounds depending on the pathophysiology of the wound process. Reports of Vinnytsia National Medical University, 28(2), 342–348. https://doi.org/10.31393/reports-vnmedical-2024-28(2)-27
- Carrasco-Labra, A., Devji, T., Qasim, A., Phillips, M. R., Wang, Y., Johnston, B. C. et al. (2021). Minimal important difference estimates for patient-reported outcomes: A systematic survey. Journal of Clinical Epidemiology, 133, 61–71. https://doi.org/10.1016/j.jclinepi.2020.11.024
- Homola, D., Kozynets, G. (2025). Modern Approaches to the Surgical Treatment of Complicated Wounds Considering Innovative Technologies and European Experience (Literature Review). Family Medicine. European Practices, 2, 108–116. https://doi.org/10.30841/2786-720x.2.2025.332008
- Reinboldt‐Jockenhöfer, F., Babadagi, Z., Hoppe, H., Risse, A., Rammos, C., Cyrek, A. et al. (2021). Association of wound genesis on varying aspects of health‐related quality of life in patients with different types of chronic wounds: Results of a cross‐sectional multicentre study. International Wound Journal, 18 (4), 432–439. https://doi.org/10.1111/iwj.13543
- World Health Organization. (2020). Access to palliative care and pain relief. Retrieved from https://www.who.int/news-room/fact-sheets/detail/palliative-care
- Eckert, K. A., Fife, C. E., Carter, M. J. (2023). The Impact of Underlying Conditions on Quality-of-Life Measurement Among Patients with Chronic Wounds, as Measured by Utility Values: A Review with an Additional Study. Advances in Wound Care, 12 (12), 680–695. https://doi.org/10.1089/wound.2023.0098
- Sen, C. K. (2023). Human Wound and Its Burden: Updated 2022 Compendium of Estimates. Advances in Wound Care, 12 (12), 657–670. https://doi.org/10.1089/wound.2023.0150
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Dmytro Homola, Georgiy Kozynets

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








