Breast implants malposition prevention after aesthetic augmentation mammoplasty
DOI:
https://doi.org/10.15587/2519-4798.2023.293393Keywords:
breast implants malposition, prevention, women's physique, implant volumeAbstract
Prevention of breast implant malposition (BIM) after submuscular augmentation mammoplasty (SAMP) for hypomastia is an actual problem, as 4.7–5.2 % of women after primary SAMP and approximately 10 % after repeated SAMP require revision surgery due to this complication.
The aim. To determine the effectiveness of prevention of BIM after SAMP by choosing the implant volume depending on the physique of women.
Materials and methods. In 112 women, the choice of implant volume for SAMP was carried out in accordance with the High Five approach – the comparison group (Group C), in 46 women according to the developed algorithm – the main group (Group M). The algorithm took into account the risk of BIM in women of different physique depending on the implant volume. If a woman insisted on having a larger implant than was calculated, an additional internal bra was created.
One year after SAMP, the amount of BIM was assessed according to the developed methodology, according to which BIM was characterised by the percentage increase in the area of the neo-osseous in relation to the area of the prosthesis. The following categories of BIM were distinguished: absent (insignificant) 1.5 % to 6.4 %, mild – 6.5 % to 10.4 %, moderate – 10.5 % to 20.0 %, significant – more than 20 %. Women's body type was assessed by the Pignet’s Index, which distinguished three categories: strong <16, medium 16–25, and weak 26–35. In group M, the maximum possible implant volume with a low risk of BIM was considered to be for women with a weak physique – 360 ml, medium – 430 ml, strong – 650 ml.
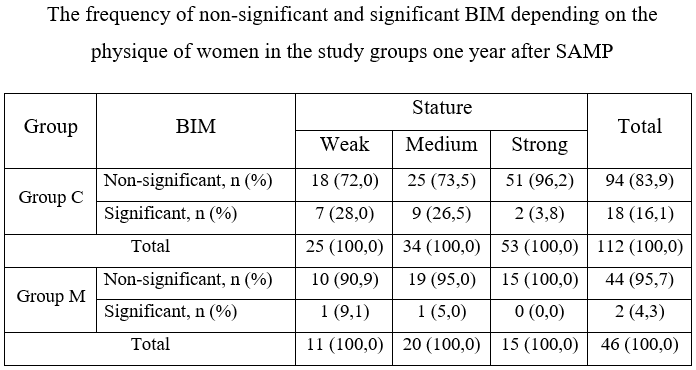
Results The mean percentage of BIM was significantly lower in group M (7.2±1.8 %) compared to group C (9.1±6.1 %), p=0.036. At the same time, the incidence of significant BIM significantly decreased from 18 (16.1 %) in group C to 2 (4.3 %) in group M, p=0.044. Moreover, patients in group M had BIM that could be classified as moderate, while in group P, 9 (50 %) women had moderate and 9 significant BIM. In the case of additional creation of an internal bra, there was no significant BIM in any case, the average value of this indicator was 6.3±1.6 % (no or mild BIM).
Conclusion. The developed personalised approach to the choice of implant volume, taking into account the physique of women, significantly improves the results of SAMP and prevents significant BIM
References
- Hidalgo, D. A., Spector, J. A. (2014). Breast Augmentation. Plastic & Reconstructive Surgery, 133 (4), 567e–583e. doi: https://doi.org/10.1097/prs.0000000000000033
- An, J., Yu, L. (2020). Advancement of Complications Related to Augmentation Mammoplasty using Silicone Gel Prosthesis. Chinese Journal of Plastic and Reconstructive Surgery, 2 (1), 51–58. doi: https://doi.org/10.1016/s2096-6911(21)00009-1
- Maxwell, G. P., Van Natta, B. W., Bengtson, B. P., Murphy, D. K. (2015). Ten-Year Results From the Natrelle 410 Anatomical Form-Stable Silicone Breast Implant Core Study. Aesthetic Surgery Journal, 35 (2), 145–155. doi: https://doi.org/10.1093/asj/sju084
- McGuire, P., Reisman, N. R., Murphy, D. K. (2017). Risk Factor Analysis for Capsular Contracture, Malposition, and Late Seroma in Subjects Receiving Natrelle 410 Form-Stable Silicone Breast Implants. Plastic & Reconstructive Surgery, 139 (1), 1–9. doi: https://doi.org/10.1097/prs.0000000000002837
- Strasser, E. (2006). Results of subglandular versus subpectoral augmentation over time: One surgeon’s observations. Aesthetic Surgery Journal, 26 (1), 45–50. doi: https://doi.org/10.1016/j.asj.2005.11.007
- Susak, Y. M., Mohammad, А. В. І. (2023). Breast implant volume as a risk factor malposition after mammoplasty augmentation in women with different body types. Prospects and innovations of science, 15 (33), 1276–1291 doi: https://doi.org/10.52058/2786-4952-2023-15(33)-1276-1291
- Susak, Y. M., Mohammad, А. B. І. (2023). Quantitative assessment of the breast implant malposition after augmentation mammaplasty. General Surgery, 2, 47–53. doi: https://doi.org/10.30978/gs-2023-2-47
- Makarycheva, V. V. (2016). The Information-Computer System Assessment of Physical Health Component. Control Systems and Computers, 1 (261), 81–91. doi: https://doi.org/10.15407/usim.2016.01.081
- Tebbetts, J. B., Adams, W. P. (2005). Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plastic and Reconstructive Surgery, 116 (7), 2005–2016.
- World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects (2013). JAMA, 310 (20), 2191–2194. doi: https://doi.org/10.1001/jama.2013.281053
- Mishalov, V. G., Khrapach, V. V., Markulan, L. Yu., Khrapach, O. V., Zakhartseva, O. I. (2018). Rotation of mammary implants one year after the primary augmentic mammary plastic surgery. Surgery of Ukraine, 1, 70–74. doi: https://doi.org/10.30978/su2018170
- Denney, B. D., Cohn, A. B., Bosworth, J. W., Kumbla, P. A. (2021). Revision Breast Augmentation. Seminars in Plastic Surgery, 35 (2), 98–109. doi: https://doi.org/10.1055/s-0041-1727272
- Brown, M. H., Somogyi, R. B., Aggarwal, S. (2016). Secondary Breast Augmentation. Plastic & Reconstructive Surgery, 138 (1), 119e–135e. doi: https://doi.org/10.1097/prs.0000000000002280
- Munhoz, A. M., de Azevedo Marques Neto, A., Maximiliano, J. (2022). Reoperative Augmentation Mammoplasty: An Algorithm to Optimize Soft-Tissue Support, Pocket Control, and Smooth Implant Stability with Composite Reverse Inferior Muscle Sling (CRIMS) and its Technical Variations. Aesthetic Plastic Surgery, 46 (3), 1116–1132. doi: https://doi.org/10.1007/s00266-021-02726-1
- Mihalečko, J., Boháč, M., Danišovič, Ľ., Koller, J., Varga, I., Kuniaková, M. (2022). Acellular Dermal Matrix in Plastic and Reconstructive Surgery. Physiological Research, 71 (1), S51–S57. doi: https://doi.org/10.33549/physiolres.935045
- Handel, N. (2013). The Double-Bubble Deformity. Plastic and Reconstructive Surgery, 132 (6), 1434–1443. doi: https://doi.org/10.1097/01.prs.0000434405.91316.96
- Chopra, K., Gowda, A. U., Kwon, E., Eagan, M., Grant Stevens, W. (2016). Techniques to Repair Implant Malposition after Breast Augmentation: A Review. Aesthetic Surgery Journal, 36 (6), 660–671. doi: https://doi.org/10.1093/asj/sjv261
- Gabriel, A., Maxwell, G. P. (2021). Treatment of Implant Malposition. Managing Common and Uncommon Complications of Aesthetic Breast Surgery. Springer, 35–44. doi: https://doi.org/10.1007/978-3-030-57121-4_4
- Castello, M. F., Silvestri, A., Nicoli, F., Dashti, T., Han, S., Grassetti, L. et al. (2014). Augmentation Mammoplasty/Mastopexy: Lessons Learned from 107 Aesthetic Cases. Aesthetic Plastic Surgery, 38 (5), 896–907. doi: https://doi.org/10.1007/s00266-014-0388-1
- Adams, W. P., Mckee, D. (2016). Matching the Implant to the Breast: A Systematic Review of Implant Size Selection Systems for Breast Augmentation. Plastic & Reconstructive Surgery, 138 (5), 987–994. doi: https://doi.org/10.1097/prs.0000000000002623
- Namnoum, J. D., Largent, J., Kaplan, H. M., Oefelein, M. G., Brown, M. H. (2013). Primary breast augmentation clinical trial outcomes stratified by surgical incision, anatomical placement and implant device type. Journal of Plastic, Reconstructive & Aesthetic Surgery, 66 (9), 1165–1172. doi: https://doi.org/10.1016/j.bjps.2013.04.046
- Munhoz, A. M., Neto, A. M., Ferrari, O. (2019). Single-Stage Augmentation Mastopexy With Composite Reverse Inferior Muscle Sling Technique for Autologous Reinforcement of the Inferior Pole: Technical Refinements and Outcomes. Aesthetic Surgery Journal, 40 (6), 356–373. doi: https://doi.org/10.1093/asj/sjz334
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Ali Bassam Ibrahim Mohammad, Yaroslav Susak

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








