Body mass index, lipid profile, and endothelial dysfunction gene polymorphism in women with early-onset and late-onset preeclampsia
DOI:
https://doi.org/10.15587/2519-4798.2024.298563Keywords:
preeclampsia, lipids, body weight, genetic thrombophilia, pregnancy complications, prognosis, gene polymorphismAbstract
The aim: to investigate and analyze clinical parameters, laboratory biomarkers of lipid metabolism and endothelial dysfunction gene polymorphisms in early-onset and late-onset preeclampsia and to identify potential risk factor(s) for the development of early-onset preeclampsia.
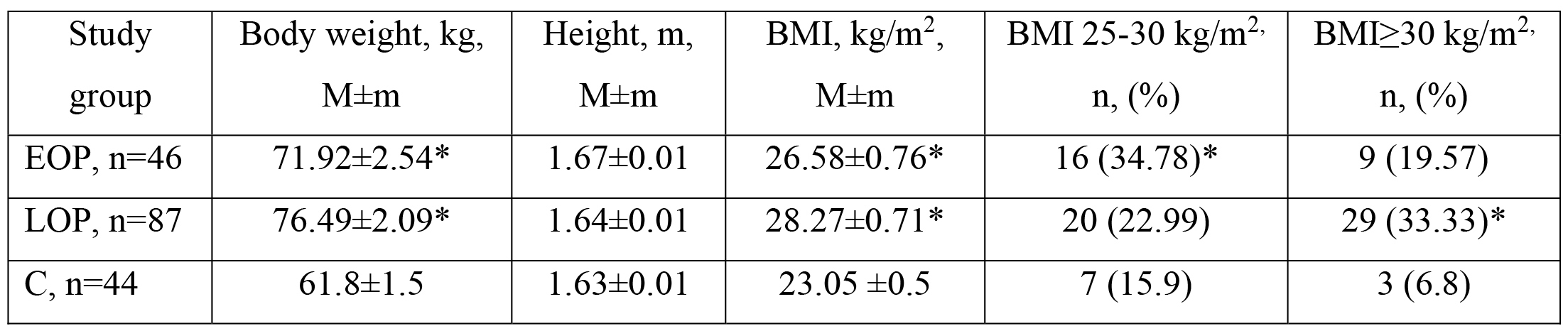
Materials and methods: a prospective case-control study included 133 women in the second half of pregnancy, including 46 with early-onset (EOP) and 87 with late-onset preeclampsia (LOP) and 34 conditionally healthy pregnant women with an uncomplicated obstetric history and no risk factors for preeclampsia. Concentrations of total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides in blood plasma were determined. Genetic polymorphisms of endothelial dysfunction (192 Q→R PON-1, 677 C→ T MTHFR) were studied using allele-specific polymerase chain reaction.
Results: Early-onset preeclampsia is associated with an increased relative risk: preterm delivery by 2.08 times (95 % CI 1.48-2.93), operative delivery by 2.2 times (95 % CI 1.46-3.33), early operative delivery by 2.9 times (95 % CI 1.5-5.5), fetal distress during delivery by 3.78 times (95 % CI 1.2-11.9), a low score on the Apgar scale on the 1st minute, less than 6 points, by 2.59 times (95 % CI 1.84-3.66), on the 5th minute – 5.04 times (95 % CI 1.41-18.11), Grade III prematurity – 13.24 times (95 % CI 3.14-55.78) compared to women with late-onset preeclampsia. The study found that overweight was more often observed in patients with EOP (34.8 %) than in those with normal pregnancy (15.9 %) (p=0.02; OR=2.8; 95 % CI 1.03-7.7), obesity (BMI > 30 kg/m2) was more often recorded in those with LOP (33.33 %) than in the control group (3 (6.8 %)) (p=0.02; OR=6.8; 95 % CI 1.9-23.9). Patients in both groups with preeclampsia showed signs of dyslipidemia, but its significance in the development of early-onset or late-onset preeclampsia has not been separately proven. The study found that the number of carriers of MTHFR 677 TT in the group with EOP prevailed over the indicator of C group where there were no carriers of the pathological homozygote 677TT (p<0.05, OR= 20.73 95 % CI 1.16-371.28), and the T allele in the EOP group occurs 1.78 times more often than in the LOP group (p<0.05, OR=2.22; 95 % CI 1.26-3.88) and 2.43 times more often than in the C group (P<0.05, or= 3.15; 95 % CI 1.54-6.45).
Conclusions: Factors of early onset of PE include pre-pregnancy, overweight, first pregnancy, a history of preeclampsia, and carrier of the 677T allele of the MTHFR gene
References
- Wójtowicz, A., Zembala-Szczerba, M., Babczyk, D., Kołodziejczyk-Pietruszka, M., Lewaczyńska, O., Huras, H. (2019). Early- and Late-Onset Preeclampsia: A Comprehensive Cohort Study of Laboratory and Clinical Findings according to the New ISHHP Criteria. International Journal of Hypertension, 2019, 1–9. https://doi.org/10.1155/2019/4108271
- Stan zdorovia zhinochoho naselennia v Ukraini za 2015–2020–2021 roky (za danymy zakladiv okhorony zdorovia sfery upravlinnia MOZ Ukrainy na terytoriiakh, shcho pidkontrolni Ukraini) (2022). Kyiv, 136.
- Tranquilli, A. L., Brown, M. A., Zeeman, G. G., Dekker, G., Sibai, B. M. (2013). The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health, 3 (1), 44–47. https://doi.org/10.1016/j.preghy.2012.11.001
- Li, X. L., Guo, P. L., Xue, Y., Gou, W. L., Tong, M., & Chen, Q. (2016). An analysis of the differences between early and late preeclampsia with severe hypertension. Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health, 6 (1), 47–52. https://doi.org/10.1016/j.preghy.2015.12.003
- Tesfa, E., Nibret, E., Munshea, A. (2020). Maternal lipid profile and risk of pre-eclampsia in African pregnant women: A systematic review and meta-analysis. PLOS ONE, 15 (12), e0243538. https://doi.org/10.1371/journal.pone.0243538
- Brown, M. A., Magee, L. A., Kenny, L. C., Karumanchi, S. A., McCarthy, F. P., Saito, S. et al. (2018). Hypertensive Disorders of Pregnancy: ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension, 72 (1), 24–43. https://doi.org/10.1161/hypertensionaha.117.10803
- He, B., Liu, Y., Maurya, M. R., Benny, P., Lassiter, C., Li, H. et al. (2021). The maternal blood lipidome is indicative of the pathogenesis of severe preeclampsia. Journal of Lipid Research, 62, 100118. https://doi.org/10.1016/j.jlr.2021.100118
- Zhou, A., Xiong, C., Hu, R., Zhang, Y., Bassig, B. A., Triche, E. et al. (2015). Pre-Pregnancy BMI, Gestational Weight Gain, and the Risk of Hypertensive Disorders of Pregnancy: A Cohort Study in Wuhan, China. PLOS ONE, 10 (8), e0136291. https://doi.org/10.1371/journal.pone.0136291
- Hogan, J. L., Anglim, B., O’Dwyer, V., Farah, N., Stuart, B., Turner, M. J. (2012). Body mass index and hypertensive disorders of pregnancy. Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health, 2 (1), 28–31. https://doi.org/10.1016/j.preghy.2011.09.003
- Kaur, D. B., Nidhi, D., Fayyaz, D. S. (2019). Study of serum lipid profile in pregnancy and its correlation with preeclampsia. Obstetrics & Gynecology International Journal, 10 (3), 169–174. https://doi.org/10.15406/ogij.2019.10.00439
- Trivett, C., Lees, Z. J., Freeman, D. J. (2021). Adipose tissue function in healthy pregnancy, gestational diabetes mellitus and pre-eclampsia. European Journal of Clinical Nutrition, 75 (12), 1745–1756. https://doi.org/10.1038/s41430-021-00948-9
- Priyanka S., B. P., Padma Vijayasree, A., Devraj, J. P., Santosh Kumar, B., Mummadi, M. K., Boiroju, N. K. (2019). A study of serum lipid profile in normal pregnancy and pregnancy induced hypertensive disorders: a case-control study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 8 (5), 2071. https://doi.org/10.18203/2320-1770.ijrcog20191969
- Rayes, B., Ardissino, M., Slob, E. A. W., Patel, K. H. K., Girling, J., Ng, F. S. (2023). Association of Hypertensive Disorders of Pregnancy With Future Cardiovascular Disease. JAMA network open, 6 (2), e230034. https://doi.org/10.1001/jamanetworkopen.2023.0034
- Froese, D. S., Huemer, M., Suormala, T., Burda, P., Coelho, D., Guéant, J.-L. et al. (2016). Mutation Update and Review of Severe Methylenetetrahydrofolate Reductase Deficiency. Human Mutation, 37 (5), 427–438. https://doi.org/10.1002/humu.22970
- Di Renzo, L., Marsella, L. T., Sarlo, F., Soldati, L., Gratteri, S., Abenavoli, L., De Lorenzo, A. (2014). C677T gene polymorphism of MTHFR and metabolic syndrome: response to dietary intervention. Journal of Translational Medicine, 12 (1). https://doi.org/10.1186/s12967-014-0329-4
- Kaur, L., Puri, M., Pal Sachdeva, M., Mishra, J., Nava Saraswathy, K. (2021). Maternal one carbon metabolism and interleukin-10 &-17 synergistically influence the mode of delivery in women with Early Onset Pre-Eclampsia. Pregnancy Hypertension, 24, 79–89. https://doi.org/10.1016/j.preghy.2021.02.011
- Huang, L. L., Tong, J. R., Huang, Y., Wei, Y. N., Chen, H. F., Chen, Y. et al. (2023). Association of MTHFR gene C677T polymorphism with pregnancy outcome. European review for medical and pharmacological sciences, 27 (1), 166–171. https://doi.org/10.26355/eurrev_202301_30868
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Tetiana Loskutova, Albina Petulko, Yuliya Donskaya

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








