Postsurgical pain intensity in children on the VAS and FLACC scale across various analgesic techniques. Mathematical prediction as a component of justification
DOI:
https://doi.org/10.15587/2519-4798.2024.301990Keywords:
local anesthetics, pain, regional analgesia, mathematical predictionAbstract
Nowadays, in pediatric practice, the Visual Analogue Scale (VAS) and the Face, Legs, Activity, Cry, Consolability (FLACC) scale are effective for assessing postsurgical pain. The modern concept of pain management includes a multimodal approach, including regional analgesia techniques.
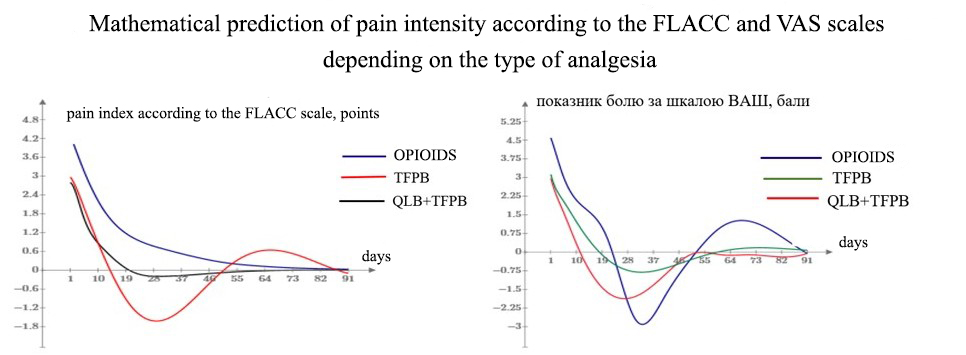
The aim of the study was to present a mathematical model to assess the efficacy of regional analgesia techniques in managing postsurgical pain intensity on the VAS and FLACC scale up to the fifth day of the study and predict the behaviour of the experimental data function up to day 87 following surgery using the autoregressive probability model.
Materials and Methods. 89 patients operated on the anterior abdominal wall were divided into 3 groups depending on the type of anesthesia. The assessment of pain management quality and the presence of acute pain was conducted using the VAS and FLACC scale on days 1, 2, 3, and 5 post-operatively in all children. The ‘predict’ function in РТС MathCad Prime 7.0. software was used to automate calculating predictions based on the Burg method.
Results. Studying the efficiency of the proposed treatment using regional analgesia techniques versus conventional analgesia enabled the prediction of varying postsurgical pain intensities on the VAS and FLACC scale based on their mathematical models, with coefficient of determination R2=0.9876, R2= 0, 9827, R2=0.9952 for the FLACC scale and R2=0.9868, R2=0,915, R2=0.9774 for the VAS.
Conclusions. The use of regional analgesia techniques in children undergoing anterior abdominal wall surgery has been confirmed to be associated with a significant reduction in postsurgical pain intensity to the fifth day of observation and predicted to remain so up to day 87
References
- Gilhus, N. E., Deuschl, G. (2019). Neuroinflammation – a common thread in neurological disorders. Nature Reviews Neurology, 15 (8), 429–430. https://doi.org/10.1038/s41582-019-0227-8
- Serhan, C. N., Gupta, S. K., Perretti, M., Godson, C., Brennan, E., Li, Y. et al. (2020). The Atlas of Inflammation Resolution (AIR). Molecular Aspects of Medicine, 74, 100894. https://doi.org/10.1016/j.mam.2020.100894
- Semkovych, Ya., Dmytriiev, D., Dobrovanov, O., Vidiscak, M., Supinova, M. (2022). Acute and chronic pain in children. A modern view of the issue. Lekársky Obzor, 71 (9), 338–342.
- Borsook, D., Youssef, A. M., Simons, L., Elman, I., Eccleston, C. (2018). When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain, 159 (12), 2421–2436. https://doi.org/10.1097/j.pain.0000000000001401
- Reust, C., Williams, A. (2016). Acute abdominal pain in children. American Family Physician, 93 (10), 830–836.
- Linton, S. J., Shaw, W. S. (2011). Impact of Psychological Factors in the Experience of Pain. Physical Therapy, 91 (5), 700–711. https://doi.org/10.2522/ptj.20100330
- Dmytriiev, D. (2018). Assessment and treatment of postoperative pain in children. Anaesthesia, Pain & Intensive Care, 22 (3), 392–400.
- Semkovych, Ya., Dmytriiev, D., Rusak, P., Zaporozhan, S., Nazarchuk, O. (2022). Prevalence of chronic pain after herniorrhaphy, orchiopexy, and bernardi procedure in children. A retrospective-prospective study. Paediatric Surgery. Ukraine, 3 (76), 8–18. https://doi.org/10.15574/ps.2022.76.8
- Hejr, H., Alizadeh, Z., Paymard, A., Khalili, A. (2017). A systematic review of pain assessment method in children. Annals of Tropical Medicine and Public Health, 10 (4), 847–849. https://doi.org/10.4103/atmph.atmph_155_17
- Verstraete, J., Ramma, L., Jelsma, J. (2020). Validity and reliability testing of the Toddler and Infant (TANDI) Health Related Quality of Life instrument for very young children. Journal of Patient-Reported Outcomes, 4 (1). https://doi.org/10.1186/s41687-020-00251-4
- Tamvaki, E., Efstratiou, F., Nteli, C., Matziou, V., Pavlopoulou, I., Myrianthefs, P. et al. (2020). Validation of the Greek Version of Comfort-B, FLACC, and BPS Scales in Critically Ill Children and Their Association with Clinical Severity. Pain Management Nursing, 21 (5), 468–475. https://doi.org/10.1016/j.pmn.2019.10.004
- Birnie, K. A., Hundert, A. S., Lalloo, C., Nguyen, C., Stinson, J. N. (2018). Recommendations for selection of self-report pain intensity measures in children and adolescents: a systematic review and quality assessment of measurement properties. Pain, 160 (1), 5–18. https://doi.org/10.1097/j.pain.0000000000001377
- Subramaniam, S. D., Doss, B., Chanderasekar, L. D., Madhavan, A., Rosary, A. M. (2018). Scope of physiological and behavioural pain assessment techniques in children – a review. Healthcare Technology Letters, 5 (4), 124–129. Portico. https://doi.org/10.1049/htl.2017.0108
- de Tovar, C., von Baeyer, C. L., Wood, C., Alibeu, J.-P., Houfani, M., Arvieux, C. (2010). Postoperative Self-Report of Pain in Children: Interscale Agreement, Response to Analgesic, and Preference for a Faces Scale and a Visual Analogue Scale. Pain Research and Management, 15 (3), 163–168. https://doi.org/10.1155/2010/475907
- Peng, T., Qu, S., Du, Z., Chen, Z., Xiao, T., Chen, R. (2023). A Systematic Review of the Measurement Properties of Face, Legs, Activity, Cry and Consolability Scale for Pediatric Pain Assessment. Journal of Pain Research, 16, 1185–1196. https://doi.org/10.2147/jpr.s397064
- Beltramini, A., Milojevic, K., Pateron, D. (2017). Pain Assessment in Newborns, Infants, and Children. Pediatric Annals, 46 (10), 387–395. https://doi.org/10.3928/19382359-20170921-03
- Merkel, S. I., Voepel-Lewis, T., Shayevitz, J. R., Malviya, S. (1997). The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatric Nursing, 23 (3), 293–297.
- Crellin, D., Sullivan, T. P., Babl, F. E., O’sullivan, R., Hutchinson, A. (2007). Analysis of the validation of existing behavioral pain and distress scales for use in the procedural setting. Pediatric Anesthesia, 17 (8), 720–733. https://doi.org/10.1111/j.1460-9592.2007.02218.x
- von Baeyer, C. L., Spagrud, L. J. (2007). Systematic review of observational (behavioral) measures of pain for children and adolescents aged 3 to 18 years. Pain, 127 (1), 140–150. https://doi.org/10.1016/j.pain.2006.08.014
- Crellin, D. J., Harrison, D., Santamaria, N., Babl, F. E. (2015). Systematic review of the Face, Legs, Activity, Cry and Consolability scale for assessing pain in infants and children. Pain, 156 (11), 2132–2151. https://doi.org/10.1097/j.pain.0000000000000305
- Matsuishi, Y., Hoshino, H., Shimojo, N., Enomoto, Y., Kido, T., Hoshino, T. et al. (2018). Verifying the validity and reliability of the Japanese version of the Face, Legs, Activity, Cry, Consolability (FLACC) Behavioral Scale. PLOS ONE, 13 (3), e0194094. https://doi.org/10.1371/journal.pone.0194094
- Kehlet, H., Jensen, T. S., Woolf, C. J. (2006). Persistent postsurgical pain: risk factors and prevention. The Lancet, 367 (9522), 1618–1625. https://doi.org/10.1016/s0140-6736(06)68700-x
- Semkovych, Y., Dmytriiev, D. (2023). Prevention of hyperalgesia in children when using various anesthesia techniques. Neonatology, Surgery and Perinatal Medicine, 13 (2 (48)), 71–77. https://doi.org/10.24061/2413-4260.xiii.2.48.2023.10
- Merella, F., Canchi-Murali, N., Mossetti, V. (2019). General principles of regional anaesthesia in children. BJA Education, 19 (10), 342–348. https://doi.org/10.1016/j.bjae.2019.06.003
- Blanco, R., Ansari, T., Riad, W., Shetty, N. (2016). Quadratus Lumborum Block Versus Transversus Abdominis Plane Block for Postoperative Pain After Cesarean Delivery: a randomized controlled trial. Regional Anesthesia and Pain Medicine, 41(6), 757–762. https://doi.org/10.1097/aap.0000000000000495
- Ishio, J., Komasawa, N., Kido, H., Minami, T. (2017). Evaluation of ultrasound-guided posterior quadratus lumborum block for postoperative analgesia after laparoscopic gynecologic surgery. Journal of Clinical Anesthesia, 41, 1–4. https://doi.org/10.1016/j.jclinane.2017.05.015
- Semkovych, Y. (2023). Impact of the CD40-CD40L system on pain severity in children after anterior abdominal wall surgery using various anaesthesia techniques. Emergency Medicine, 19 (6), 414–418. https://doi.org/10.22141/2224-0586.19.6.2023.1621
- Ahiskalioglu, A., Aydin, M. E., Doymus, O., Yayik, A. M., Celik, E. C. (2019). Ultrasound guided transversalis fascia plane block for lower abdominal surgery: First pediatric report. Journal of Clinical Anesthesia, 55, 130–131. https://doi.org/10.1016/j.jclinane.2018.12.046
- El-Boghdadly, K., Elsharkawy, H., Short, A., Chin, K. J. (2016). Quadratus Lumborum Block Nomenclature and Anatomical Considerations. Regional Anesthesia and Pain Medicine, 41 (4), 548–549. https://doi.org/10.1097/aap.0000000000000411
- Berde, C. (2004). Local anesthetics in infants and children: an update. Pediatric Anesthesia, 14 (5), 387–393. https://doi.org/10.1111/j.1460-9592.2004.01336.x
- Yaster, M., Tobin, J. R., Fisher, Q. A., Maxwell, L. G. (1994). Local anesthetics in the management of acute pain in children. The Journal of Pediatrics, 124 (2), 165–176. https://doi.org/10.1016/s0022-3476(94)70300-0
- Mazoit, J. (2011). Local anesthetics and their adjuncts. Pediatric Anesthesia, 22 (1), 31–38. https://doi.org/10.1111/j.1460-9592.2011.03692.x
- Suresh, S., Ecoffey, C., Bosenberg, A., Lonnqvist, P.-A., de Oliveira, G. S., de Leon Casasola, O. et al. (2018). The European Society of Regional Anaesthesia and Pain Therapy/American Society of Regional Anesthesia and Pain Medicine Recommendations on Local Anesthetics and Adjuvants Dosage in Pediatric Regional Anesthesia. Regional Anesthesia and Pain Medicine, 43 (2), 211–216. https://doi.org/10.1097/aap.0000000000000702
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Yaroslav Semkovych

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








