Assessment of interalveolar height deficiency using computed tomography in patients with TMJ dysfunction in articulation-occlusion disorders
DOI:
https://doi.org/10.15587/2519-4798.2024.315966Keywords:
cone-beam computed tomography, temporomandibular joint dysfunction, occlusal and articulation disorders, interalveolar heightAbstract
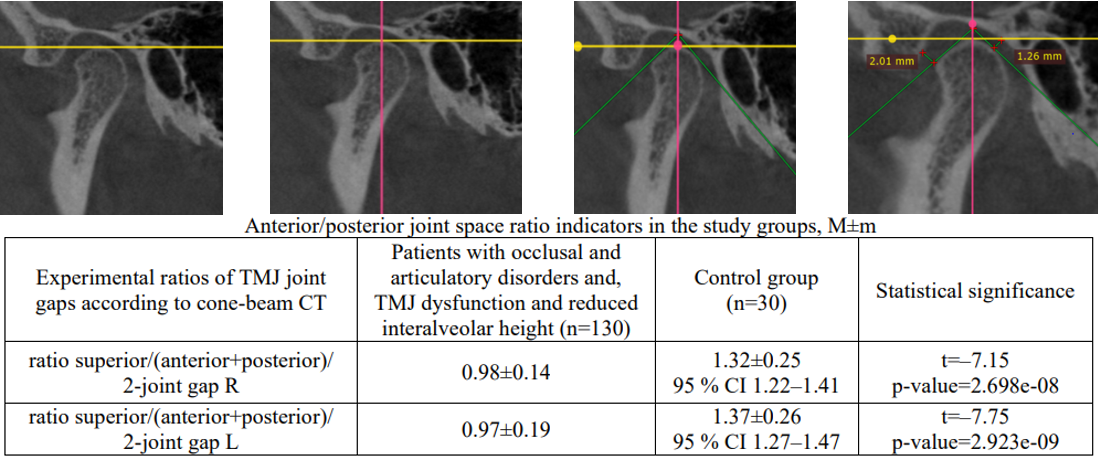
This article reviews the assessment of interalveolar height deficit in morphometric comparison with its projection onto the superior space of the temporomandibular joint (TMJ) using cone-beam computed tomography (CT) of the TMJ. The technique for calculating the gaps between the fossa and the head, determining the coefficients for their comparison, and their correlation with clinical signs of TMJ dysfunction in occlusal and articulatory disorders is described.
The aim - to determine CT diagnostic criteria for decreased interalveolar height in patients with functional TMJ disorders with occlusal and articulatory disorders at the stage of orthopedic treatment planning.
Materials and research methods. An examination was conducted of 150 patients with functional disorders of the chewing apparatus and occlusal disorders, who were included in the experimental group and 30 practically healthy individuals - the control group. Both groups were comparable in age and sex. Cone-beam tomography was performed on the MyRay Hyperion X9 PRO model with iRYS 16.3.1 software. During the clinical dental examination, the occlusion of the dentition was assessed, the reduction of the interalveolar height was determined, the width of the mouth opening was assessed, the mobility of the lower jaw was assessed, the symmetry of the mouth opening was determined, clicking and crunching in the TMJ were determined.
Research result. When analyzing cone-beam tomography data, interalveolar height deficiency was classified as a decrease in the proposed coefficient for assessing the size of the upper TMJ space in at least one joint. A decrease in the specified ratio was found in 130 (86.67 %) patients with TMJ dysfunction and occlusal and articulation disorders according to CT data and confirmed by the anatomical and physiological method in 81 (54.00 %) patients, while its moderate decrease was confirmed by measurements by the topographic and physiological method (0.5-2.5 mm) in 62 (76.54 %) people and a significant decrease (more than 2.5 mm) in 19 (23.46 %) people, in 20 (13.33 %) patients, the coincidence of the absence of interalveolar height deficiency according to CT data and the anatomical and physiological method was noted.
Bilateral reduction of interalveolar height was found in 82 (54.67 %) patients of the study group; 36 (24.00 %) of them had clinically observed pain syndrome. When assessing the deficiency of interalveolar height by the topographic-physiological method, confirmation of its moderate reduction (0.5-2.5 mm) was found in 51 (62.20 %) individuals and a significant reduction (more than 2.5 mm) in 8 (9.75 %) individuals. Unilateral reduction of interalveolar height was found in 48 (32.00 %) patients of the study group; 20 (41.66 %) of them had clinically observed pain syndrome.
Conclusions. The assessment of the size of the superior articular space in comparison with the average value of the anterior and posterior articular gaps when determining their sizes using cone-beam CT of the TMJ may be a marker of decreased interalveolar height in patients with TMJ dysfunction and occlusal and articulatory disorders
References
- Bida, O., Proshchenko, A., Bida, O., Reshetnyk, L. (2024). Some aspects of the use of standard and individually modeled abutments in the prosthetic rehabilitation of patients with partial tooth loss with orthopedic structures based on dental implants. Stomatological Bulletin, 126 (1), 156–161. https://doi.org/10.35220/2078-8916-2024-51-1.26
- List, T., Wahlund, K., Wenneberg, B., Dworkin, S. F. (1999). TMD in children and adolescents: prevalence of pain, gender differences, and perceived treatment need. Journal of orofacial pain, 13 (1), 9–20.
- Magnusson, T., Egermark, I., Carlsson, G. E. (2005). A prospective investigation over two decades on signs and symptoms of temporomandibular disorders and associated variables. A final summary. Acta Odontologica Scandinavica, 63 (2), 99–109. https://doi.org/10.1080/00016350510019739
- De Boever, J. A., Carlsson, G. E., Klineberg, I. J. (2000). Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Journal of Oral Rehabilitation, 27 (8), 647–659. https://doi.org/10.1046/j.1365-2842.2000.00623.x
- Johansson, A., Johansson, A. ‐K., Omar, R., Carlsson, G. E. (2008). Rehabilitation of the worn dentition. Journal of Oral Rehabilitation, 35 (7), 548–566. Portico. https://doi.org/10.1111/j.1365-2842.2008.01897.x
- Proschenko, A. M., Proschenko, N. S., Reshetnyk, L. L., Zelinskaya, N. A., Chervonna, N. V., Melnychyk, T. A. (2024). Indicative features of tissue and microbial sensitization in the pathogenesis of generalized parodontitis associated with rheumatoid arthritis. Medychni Perspektyvy, 29 (2), 168–174. https://doi.org/10.26641/2307-0404.2024.2.307620
- List, T., Axelsson, S., Leijon, G. (2003). Pharmacologic interventions in the treatment of temporomandibular disorders, atypical facial pain, and burning mouth syndrome. A qualitative systematic review. Journal of orofacial pain, 17 (4), 301–310.
- Carlsson, G. E. (2009). Critical review of some dogmas in prosthodontics. Journal of Prosthodontic Research, 53 (1), 3–10. https://doi.org/10.1016/j.jpor.2008.08.003
- Dao, T. T., Lavigne, G. (1998). Oral Splints: the Crutches for Temporomandibular Disorders and Bruxism? Critical Reviews in Oral Biology & Medicine, 9 (3), 345–361. https://doi.org/10.1177/10454411980090030701
- Bida, O. V., Bida, O. V. (2023). Features of preventive measures for dental prosthetics supported by dental implants. Ukrainian Dental Almanac, 4, 23–27. https://doi.org/10.31718/2409-0255.4.2023.04
- Ormianer, Z., Palty, A. (2009). Altered vertical dimension of occlusion: a comparative retrospective pilot study of tooth- and implant-supported restorations. The International Journal of Oral & Maxillofacial Implants, 24 (3), 497–501.
- Proschenko, А. М., Proschenko, N. S., Shemelko, M. L., Reshetnyk, L. L., Chervonna, N. V., Sorokina, К. О. (2024). Assessment of the treatment quality of patients with functional disorders of the dento-magular apparatus combined with the dentoalveolar form of deep bite. Clinical and Preventive Medicine, 4, 26–32. https://doi.org/10.31612/2616-4868.4.2024.04
- Abduo, J., Lyons, K. (2012). Clinical considerations for increasing occlusal vertical dimension: a review. Australian Dental Journal, 57 (1), 2–10. https://doi.org/10.1111/j.1834-7819.2011.01640.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Andriy Proschenko

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.








