Occupational factors, life expectancy, and biotechnological and pharmacological health support strategies
DOI:
https://doi.org/10.15587/2519-8025.2025.343241Keywords:
Average life expectancy, professions, gender, prominent figuresAbstract
The aim of the study was to analyze the associations of life expectancy and professions among prominent people of different historical periods, as well as some biotechnological and pharmacological aspects of promoting longevity.
Materials and methods. The work used statistical analysis and descriptive-comparative analysis.
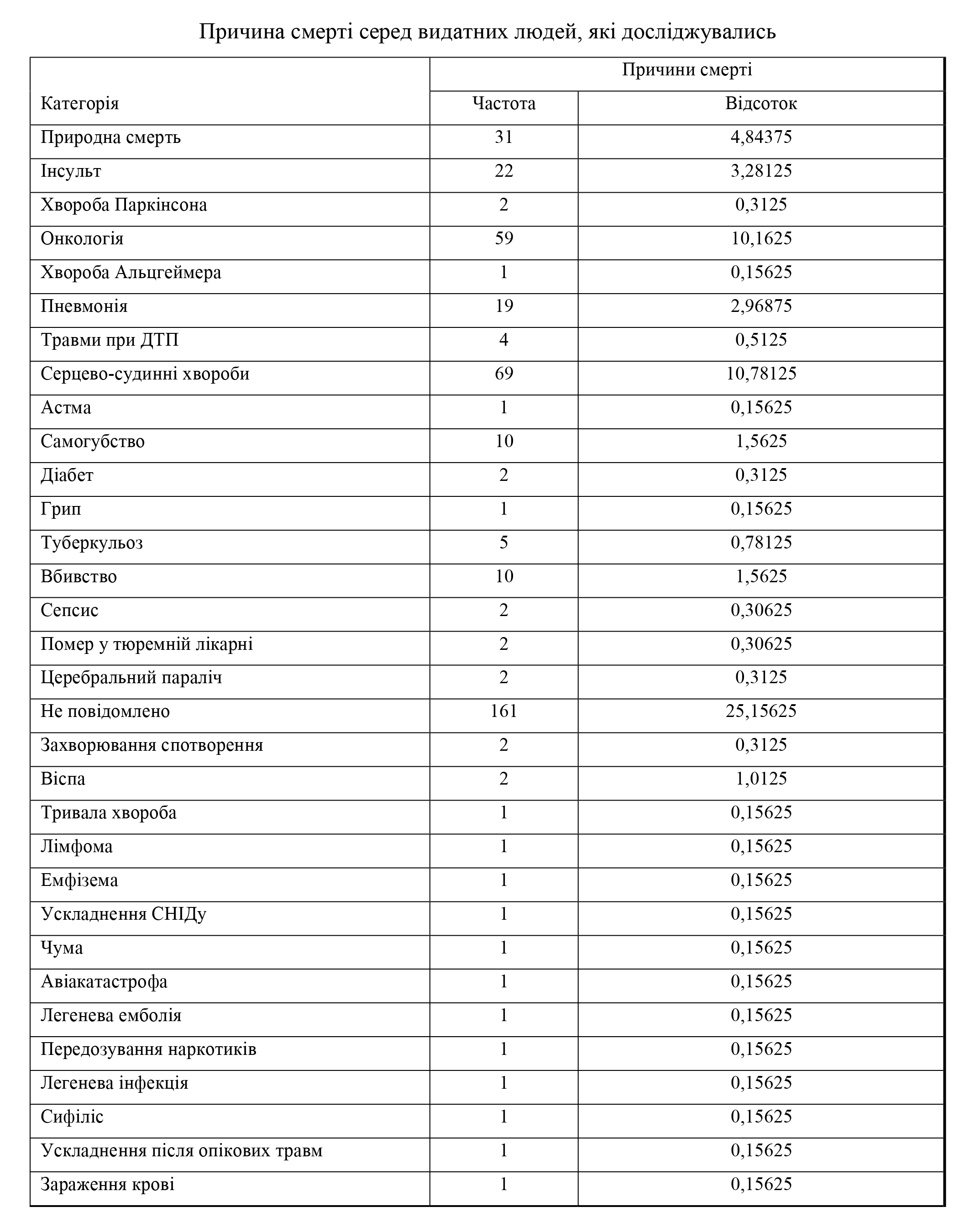
Results and discussion. The analysis of the literature shows that the average human life expectancy is a variable value. Life expectancy for the period from 1800 to 2011 increased from 30 to 68 years, in 2016 it was 69 years; for men - 67 years, for women - 71.1 years. There are significant differences in the life expectancy of a person within each country. The factors that determine the average life expectancy relate to education, income, employment and profession, as well as other indicators of socio-economic status. 640 prominent people were selected for the study, including 537 men and 103 women. Prominent people were residents of 45 countries, the largest number of people in the USA - 255, Great Britain - 65, Ukraine - 49, France - 42, Germany - 33 individuals. Prominent people were divided into a group of living (109 people) and deceased (531 people). The average life expectancy of the living is 73.4 years and this is more than the average life expectancy of the deceased, their age is 72.3 years. During the work, it has been found that there are differences in the average life expectancy within each country, between professional groups. The average life expectancy of all prominent people in the study is 72.9 years. It has been found that among the professional groups in the study, politicians have the highest average life expectancy. The results of studies of average life expectancy in the relationship between gender and professional activity showed that for men this figure is 71.4, for women - 74.8 years.
Conclusions. According to the results of the study, the average life expectancy of men is 71.9 years, and of women is 74.4 years. In the group of living people, the highest indicators of average life expectancy are programmers, and in the group of living and deceased prominent people, this indicator is highest among politicians. These data confirm scientific data on the dependence of life expectancy on gender and professional activity. In our further studies, we plan to study possible associations with diseases
References
- Slovnyk-dovidnyk z ekolohii (2013). Kherson: PP Vyshemyrskyi V. S., 226.
- Humenna, I. S., Pohorila, I. O. (2014). Tryvalist zhyttia ta problemy dovholittia. Biolohichni doslidzhennia – 2014. Zhytomyr: Vyd-vo ZhDU im. I.Franka, 320–323. Available at: http://eprints.zu.edu.ua/10971/1/І._С._Гуменна1__І._О._Погоріла2.pdf
- Doroshenko, L. S. (2005). Demohrafiia. Kyiv: MAUP, 112.
- Buzhylova, O. P. (2012). Tryvalist zhyttia na rannikh etapakh kamianoho stolittia. Biolohiia, 16/18, 102–107.
- Krysachenko, V. S. (2005). Dynamika naselennia: Populiatsiini, etnichni ta hlobalni vymiry. Kyiv: Vydavnytstvo Natsionalnoho instytutu stratehichnykh doslidzhen, 368.
- Riley, J. C. (2001). Rising life expectancy: a global history. Cambridge University Press, 243.
- Murphy, S. L., Xu, J. Q., Kochanek, K. D., Arias, E. (2018). Mortality in the United States, 2017 NCHS Data Brief, no 328. Hyattsville: National Center for Health Statistics.
- Life expectancy history. World life expectancy. Available at: http://www.worldlifeexpectancy.com/history-of-life-expectancy
- Barford, A., Dorling, D., Smith, G. D., Shaw, M. (2006). Life expectancy: women now on top everywhere. BMJ, 332 (7545), 808. https://doi.org/10.1136/bmj.332.7545.808
- Global Health Observatory. WHO. Available at: https://www.who.int/data/gho
- Rynhach, N. (2008). Problema nadsmertnosti cholovikiv v Ukraini: hendernyi analiz u derzhavnomu upravlinni okhoronoiu hromadskoho zdorovia. Stratehichni priorytety, 3, 142–148.
- Pyrozhkov, S. I. (2004). Demohrafichnyi faktor u hlobalnii stratehii rozvytku Ukrainy. Demohrafiia ta sotsialna polityka, 1-2, 5–20.
- Kurylo, I. O. (2014). Demohrafichni protsesy ta struktury v Ukraini: suchasni rehionalni osoblyvosti. Aktualni problemy rozvytku ekonomiky rehionu, 10, 141–148.
- Libanova, E. M. (Ed.) (2007). Smertnist naselennia Ukrainy u trudoaktyvnomu vitsi. Kyiv: In-t demohrafii ta sotsialnykh doslidzhen NAN Ukrainy, 211.
- Poliakov, O. A. (2001). Fiziolohichna kharakterystyka trudovoi diialnosti liudyny u vikovomu aspekti i otsinka pratsezdatnosti. [Extended abstract of Doctoral dissertation].
- Henderna rivnist i rozvytok: pohliad u konteksti yevropeiskoi stratehii Ukrainy (2016). Kyiv: Tsentr Razumkova, «ZAPOVIT», 244.
- Gendernyi parytet v umovakh rozbudovy suchasnoho ukrainskoho suspilstva (2002). Kyiv: Ukrainskyi in-t sotsialnykh doslidzhen, 121.
- Lavrynenko, N. V.; Vorona, V. M., Ruchka, A. O. (Eds.) (2000). Genderni stereotypy masovoi svidomosti. Ukrainske suspilstvo: monitorynh – 2000 r. Kyiv: I-nt sotsiolohii NAN Ukrainy.
- Wlliams, J., Best, D. (1990). Measuring Sex Stereotypes. A Multinational Study. Nebury Park: Sage Publications.
- Cui, Y., Zong, H., Yan, H., Zhang, Y. (2014). The effect of testosterone replacement therapy on prostate cancer: a systematic review and meta-analysis. Prostate Cancer and Prostatic Diseases, 17 (2), 132–143. https://doi.org/10.1038/pcan.2013.60
- Kardoust Parizi, M., Abufaraj, M., Fajkovic, H., Kimura, S., Iwata, T., D’Andrea, D. et al. (2019). Oncological safety of testosterone replacement therapy in prostate cancer survivors after definitive local therapy: A systematic literature review and meta-analysis. Urologic Oncology: Seminars and Original Investigations, 37 (10), 637–646. https://doi.org/10.1016/j.urolonc.2019.06.007
- Sokal, R. R., Rohlf, F. J. (1995). Biometry. New York: WH Freeman and company.
- Derzhavna sluzhba statystyky Ukrainy. Available at: http://www.ukrstat.gov.ua/
- Burdorf, A. (2008). The importance of solid employment for health. Scandinavian Journal of Work, Environment & Health, 34 (2), 81–82. https://doi.org/10.5271/sjweh.1216
- Toch-Marquardt, M., Menvielle, G., Eikemo, T. A., Kulhánová, I., Kulik, M. C., Bopp, M. et al. (2014). Occupational Class Inequalities in All-Cause and Cause-Specific Mortality among Middle-Aged Men in 14 European Populations during the Early 2000s. PLoS ONE, 9 (9), e108072. https://doi.org/10.1371/journal.pone.0108072
- Stringhini, S., Carmeli, C., Jokela, M., Avendaño, M., Muennig, P., Guida, F. et al. (2017). Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. The Lancet, 389 (10075), 1229–1237. https://doi.org/10.1016/s0140-6736(16)32380-7
- Ludvigsson, J. F., Almqvist, C., Bonamy, A.-K. E., Ljung, R., Michaëlsson, K., Neovius, M. et al. (2016). Registers of the Swedish total population and their use in medical research. European Journal of Epidemiology, 31 (2), 125–136. https://doi.org/10.1007/s10654-016-0117-y
- Ludvigsson, J. F., Otterblad-Olausson, P., Pettersson, B. U., Ekbom, A. (2009). The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. European Journal of Epidemiology, 24 (11), 659–667. https://doi.org/10.1007/s10654-009-9350-y
- Lozano, M., Solé-Auró, A. (2021). Happiness and life expectancy by main occupational position among older workers: Who will live longer and happy? SSM – Population Health, 13, 100735. https://doi.org/10.1016/j.ssmph.2021.100735
- van Raalte, A. A., Martikainen, P., Myrskylä, M. (2013). Lifespan Variation by Occupational Class: Compression or Stagnation Over Time? Demography, 51 (1), 73–95. https://doi.org/10.1007/s13524-013-0253-x
- de Wind, A., Sewdas, R., Hoogendijk, E. O., van der Beek, A. J., Deeg, D. J. H., Boot, C. R. L. (2020). Occupational Exposures Associated with Life Expectancy without and with Disability. International Journal of Environmental Research and Public Health, 17(17), 6377. https://doi.org/10.3390/ijerph17176377
- Järvholm, B., Reuterwall, C., Bystedt, J. (2012). Mortality attributable to occupational exposure in Sweden. Scandinavian Journal of Work, Environment & Health, 39 (1), 106–111. https://doi.org/10.5271/sjweh.3284
- Global and regional burden of disease and injury in 2016 arising from occupational exposures: a systematic analysis for the Global Burden of Disease Study 2016 (2020). Occupational and Environmental Medicine, 77 (3), 133–141. https://doi.org/10.1136/oemed-2019-106008
- Rushton, L. (2017). The Global Burden of Occupational Disease. Current Environmental Health Reports, 4 (3), 340–348. https://doi.org/10.1007/s40572-017-0151-2
- Global and regional burden of cancer in 2016 arising from occupational exposure to selected carcinogens: a systematic analysis for the Global Burden of Disease Study 2016 (2020). Occupational and Environmental Medicine, 77 (3), 151–159. https://doi.org/10.1136/oemed-2019-106012
- Carlsson, S., Andersson, T., Talbäck, M., Feychting, M. (2019). Incidence and prevalence of type 2 diabetes by occupation: results from all Swedish employees. Diabetologia, 63 (1), 95–103. https://doi.org/10.1007/s00125-019-04997-5
- Enroth, L., Veenstra, M., Aartsen, M., Kjær, A. A., Nilsson, C. J., Fors, S. (2019). Are there educational disparities in health and functioning among the oldest old? Evidence from the Nordic countries. European Journal of Ageing, 16 (4), 415–424. https://doi.org/10.1007/s10433-019-00517-x
- Fors, S., Thorslund, M. (2014). Enduring inequality: educational disparities in health among the oldest old in Sweden 1992–2011. International Journal of Public Health, 60 (1), 91–98. https://doi.org/10.1007/s00038-014-0621-3
- Enroth, L., Raitanen, J., Hervonen, A., Nosraty, L., Jylha, M. (2014). Is socioeconomic status a predictor of mortality in nonagenarians? The vitality 90+ study. Age and Ageing, 44 (1), 123–129. https://doi.org/10.1093/ageing/afu092
- Fors, S., Modin, B., Koupil, I., Vågerö, D. (2011). Socioeconomic inequalities in circulatory and all-cause mortality after retirement: the impact of mid-life income and old-age pension. Evidence from the Uppsala Birth Cohort Study. Journal of Epidemiology and Community Health, 66 (7), e16–e16. https://doi.org/10.1136/jech.2010.131177
- Lampert, T., Hoebel, J. (2018). Soziale Ungleichheit und Gesundheit im höheren Lebensalter. Zeitschrift Für Gerontologie Und Geriatrie, 52 (S1), 91–99. https://doi.org/10.1007/s00391-018-01487-y
- Cacciani, L., Bargagli, A. M., Cesaroni, G., Forastiere, F., Agabiti, N., Davoli, M. (2015). Education and Mortality in the Rome Longitudinal Study. PLOS ONE, 10 (9), e0137576. https://doi.org/10.1371/journal.pone.0137576
- Galobardes, B. (2004). Childhood Socioeconomic Circumstances and Cause-specific Mortality in Adulthood: Systematic Review and Interpretation. Epidemiologic Reviews, 26 (1), 7–21. https://doi.org/10.1093/epirev/mxh008
- Diderichsen, F., Andersen, I., Manuel, C., Andersen, A.-M. N., Bach, E., Baadsgaard, M. et al. (2012). Health Inequality – determinants and policies. Scandinavian Journal of Public Health, 40, 12–105. https://doi.org/10.1177/1403494812457734
- Kunst, A. E., Groenhof, F., Mackenbach, J. P., Leon, D. A. (1998). Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies Commentary: Unequal inequalities across Europe. BMJ, 316 (7145), 1636–1642. https://doi.org/10.1136/bmj.316.7145.1636
- Hämmig, O., Bauer, G. F. (2013). The social gradient in work and health: a cross-sectional study exploring the relationship between working conditions and health inequalities. BMC Public Health, 13 (1). https://doi.org/10.1186/1471-2458-13-1170
- Mackenbach, J. P., Stirbu, I., Roskam, A.-J. R., Schaap, M. M., Menvielle, G., Leinsalu, M., Kunst, A. E. (2008). Socioeconomic Inequalities in Health in 22 European Countries. New England Journal of Medicine, 358 (23), 2468–2481. https://doi.org/10.1056/nejmsa0707519
- Menvielle, G., Leclerc, A., Chastang, J.-F., Melchior, M., Luce, D. (2007). Changes in Socioeconomic Inequalities in Cancer Mortality Rates Among French Men Between 1968 and 1996. American Journal of Public Health, 97 (11), 2082–2087. https://doi.org/10.2105/ajph.2005.073429
- Mühlau, P. (2011). Gender Inequality and Job Quality in Europe. Management Revu, 22 (2), 114–131. https://doi.org/10.5771/0935-9915-2011-2-114
- European Commission Report on equality between women and men in the European Union (2018). Luxembourg: Publications Office of the European Union.
- Cesaroni, G., Agabiti, N., Forastiere, F., Ancona, C., Perucci, C. A. (2006). Socioeconomic differentials in premature mortality in Rome: changes from 1990 to 2001. BMC Public Health, 6 (1). https://doi.org/10.1186/1471-2458-6-270
- Kauppinen, T, Uuksulainen, S, Saalo, A, Mäkinen, I., Pukkala, E. (2014). Use of the Finnish Information System on Occupational Exposure (FINJEM) in epidemiologic, surveillance, and other applications. The Annals of Occupational Hygiene, 58, 380–396. https://doi.org/10.1093/annhyg/met074
- Deeg, D. J. H., Comijs, H. C., Hoogendijk, E. O., van der Noordt, M., Huisman, M. (2018). 23-Year Trends in Life Expectancy in Good and Poor Physical and Cognitive Health at Age 65 Years in the Netherlands, 1993–2016. American Journal of Public Health, 108 (12), 1652–1658. https://doi.org/10.2105/ajph.2018.304685
- Häkkänen, M., Viikari-Juntura, E., Martikainen, R. (2001). Job experience, work load, and risk of musculoskeletal disorders. Occupational and Environmental Medicine, 58 (2), 129–135. https://doi.org/10.1136/oem.58.2.129
- Butterworth, P., Leach, L. S., Strazdins, L., Olesen, S. C., Rodgers, B., Broom, D. H. (2011). The psychosocial quality of work determines whether employment has benefits for mental health: results from a longitudinal national household panel survey. Occupational and Environmental Medicine, 68 (11), 806–812. https://doi.org/10.1136/oem.2010.059030
- van den Berg, T. I. J., Alavinia, S. M., Bredt, F. J., Lindeboom, D., Elders, L. A. M., Burdorf, A. (2008). The influence of psychosocial factors at work and life style on health and work ability among professional workers. International Archives of Occupational and Environmental Health, 81 (8), 1029–1036. https://doi.org/10.1007/s00420-007-0296-7
- Leijten, F. R. M., van den Heuvel, S. G., van der Beek, A. J., Ybema, J. F., Robroek, S. J. W., Burdorf, A. (2014). Associations of Work-Related Factors and Work Engagement with Mental and Physical Health: A 1-Year Follow-up Study Among Older Workers. Journal of Occupational Rehabilitation, 25 (1), 86–95. https://doi.org/10.1007/s10926-014-9525-6
- Head, J., Chungkham, H. S., Hyde, M., Zaninotto, P., Alexanderson, K., Stenholm, S. et al. (2018). Socioeconomic differences in healthy and disease-free life expectancy between ages 50 and 75: a multi-cohort study. European Journal of Public Health, 29 (2), 267–272. https://doi.org/10.1093/eurpub/cky215
- Platts, L. G., Head, J., Stenholm, S., Singh Chungkham, H., Goldberg, M., Zins, M. (2016). Physical occupational exposures and health expectancies in a French occupational cohort. Occupational and Environmental Medicine, 74 (3), 176–183. https://doi.org/10.1136/oemed-2016-103804
- Magnusson Hanson, L. L., Westerlund, H., Chungkham, H. S., Vahtera, J., Rod, N. H., Alexanderson, K. et al. (2018). Job strain and loss of healthy life years between ages 50 and 75 by sex and occupational position: analyses of 64 934 individuals from four prospective cohort studies. Occupational and Environmental Medicine, 75 (7), 486–493. https://doi.org/10.1136/oemed-2017-104644
- Mathers, C. D., Robine, J. M. (1997). How good is Sullivan’s method for monitoring changes in population health expectancies? Journal of Epidemiology and Community Health, 51 (1), 80–86. https://doi.org/10.1136/jech.51.1.80
- Padkapayeva, K., Gilbert-Ouimet, M., Bielecky, A., Ibrahim, S., Mustard, C., Brisson, C., Smith, P. (2018). Gender/Sex Differences in the Relationship between Psychosocial Work Exposures and Work and Life Stress. Annals of Work Exposures and Health, 62 (4), 416–425. https://doi.org/10.1093/annweh/wxy014
- Rosenthal, L., Carroll-Scott, A., Earnshaw, V. A., Santilli, A., Ickovics, J. R. (2012). The importance of full-time work for urban adults’ mental and physical health. Social Science & Medicine, 75 (9), 1692–1696. https://doi.org/10.1016/j.socscimed.2012.07.003
- Zabkiewicz, D. (2009). The mental health benefits of work: do they apply to poor single mothers? Social Psychiatry and Psychiatric Epidemiology, 45 (1), 77–87. https://doi.org/10.1007/s00127-009-0044-2
- Martín, U., Domínguez-Rodríguez, A., Bacigalupe, A. (2019). Desigualdades sociales en salud en población mayor: una aportación desde la salud pública al debate sobre el retraso de la edad de jubilación en España. Gaceta Sanitaria, 33 (1), 82–84. https://doi.org/10.1016/j.gaceta.2017.10.010
- Solé-Auró, A., Lozano, M. (2019). Inequalities in Longevity by Education Level in Spain: A Life Satisfaction Approach. Social Indicators Research, 144 (2), 729–744. https://doi.org/10.1007/s11205-018-02057-w
- Arpino, B., Solé-Auró, A. (2017). Education Inequalities in Health Among Older European Men and Women: The Role of Active Aging. Journal of Aging and Health, 31 (1), 185–208. https://doi.org/10.1177/0898264317726390
- Cambois, E., Laborde, C., Romieu, I., Robine, J.-M. (2011). Occupational inequalities in health expectancies in France in the early 2000s: Unequal chances of reaching and living retirement in good health. Demographic Research, 25, 407–436. https://doi.org/10.4054/demres.2011.25.12
- Majer, I. M., Nusselder, W. J., Mackenbach, J. P., Kunst, A. E. (2010). Socioeconomic inequalities in life and health expectancies around official retirement age in 10 Western-European countries. Journal of Epidemiology and Community Health, 65 (11), 972–979. https://doi.org/10.1136/jech.2010.111492
- Cambois, E., Brønnum-Hansen, H., Hayward, M., Nusselder, W. J.; Jagger, C., Crimmins, E. M., Saito, Y., de Carvalho Yokota, R. T., Van Oyen, H., Robine, J. M. (Eds.) (2020). Monitoring Social Differentials in Health Expectancies. International Handbook of Health Expectancies. Cham: Springer, 45–66. https://doi.org/10.1007/978-3-030-37668-0_4
- Permanyer, I., Spijker, J., Blanes, A., Renteria, E. (2018). Longevity and Lifespan Variation by Educational Attainment in Spain: 1960–2015. Demography, 55 (6), 2045–2070. https://doi.org/10.1007/s13524-018-0718-z
- Luy, M., Wegner-Siegmundt, C., Wiedemann, A., Spijker, J. (2015). Life Expectancy by Education, Income and Occupation in Germany: Estimations Using the Longitudinal Survival Method. Comparative Population Studies, 40 (4), 339–436. https://doi.org/10.12765/cpos-2015-16
- Zaninotto, P., Batty, G. D., Stenholm, S., Kawachi, I., Hyde, M., Goldberg, M. et al. (2020). Socioeconomic Inequalities in Disability-free Life Expectancy in Older People from England and the United States: A Cross-national Population-Based Study. The Journals of Gerontology: Series A, 75 (5), 906–913. https://doi.org/10.1093/gerona/glz266
- Brønnum-Hansen, H., Foverskov, E., Andersen, I. (2019). Occupational inequality in health expectancy in Denmark. Scandinavian Journal of Public Health, 48 (3), 338–345. https://doi.org/10.1177/1403494819882138
- Klap, J., Schmid, M., Loughlin, K. R. (2015). The Relationship between Total Testosterone Levels and Prostate Cancer: A Review of the Continuing Controversy. Journal of Urology, 193 (2), 403–414. https://doi.org/10.1016/j.juro.2014.07.123
- Encyclopædia Britannica (2025). Available at: https://www.britannica.com/topic/Encyclopaedia-Britannica-English-language-reference-work
- Zar, J. H. (2010). Biostatistical Analysis. New York: Prentice Hall.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Olga Filiptsova, Olga Naboka, Oleksandr Ochkur, Nataliia Dvinskykh, Alina Soloviova, Mosiichuk Kyrylo, Oleksandra Kravtsova

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.
Authors, who are published in this journal, agree to the following conditions:
1. The authors reserve the right to authorship of the work and pass the first publication right of this work to the journal under the terms of a Creative Commons CC BY, which allows others to freely distribute the published research with the obligatory reference to the authors of the original work and the first publication of the work in this journal.
2. The authors have the right to conclude separate supplement agreements that relate to non-exclusive work distribution in the form in which it has been published by the journal (for example, to upload the work to the online storage of the journal or publish it as part of a monograph), provided that the reference to the first publication of the work in this journal is included.







