Social-pharmaceutical aspects of parents' attitudes towards children's vaccination
DOI:
https://doi.org/10.15587/2519-4852.2023.282687Keywords:
medical and pharmaceutical specialists, specialists of other specialties, parents, children, vaccination, educational professional program, curriculum, pharmacyAbstract
The aim. Study of the attitude of parents with medical and pharmaceutical and other educations to vaccination of their children from the point of view of social pharmacy.
Materials and methods. An anonymous online survey of 1,566 respondents (of whom 302 are parents with medical and pharmaceutical education) on the Google Form online service in the Viber mobile application and on the Facebook social network, which was conducted from September 16, 2021 to October 6, 2021.
Methods of analysis, synthesis and generalization were used.
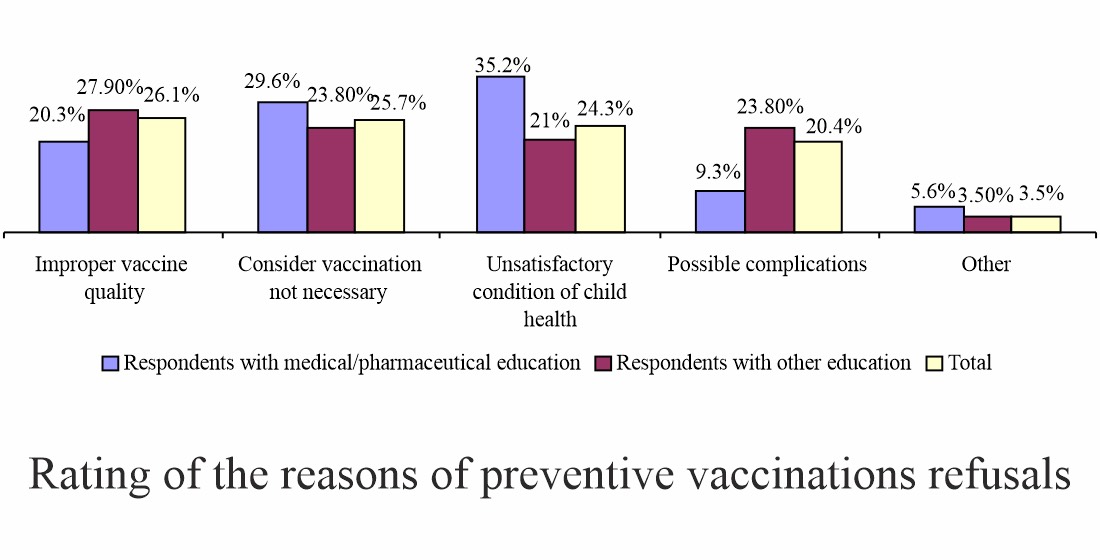
Results. A high degree of commitment to vaccination among the respondents was established (almost 9 out of 10 parents). 26.1 % of respondents motivate the refusal by the inadequate quality of vaccines, 25.7 % consider vaccination to be inappropriate; 24.3 % do not administer preventive vaccinations to children due to their unsatisfactory state of health; 20.4 % - due to possible side reactions. 67.1 % of parents are interested in the composition of vaccines, 95.6 % know the symptoms and complications of the diseases for which vaccination is carried out, and 96.6 % - side effects after vaccination, although 74.5 % want to receive more information about possible complications. At the same time, there are slightly fewer supporters of vaccination among respondents with medical and pharmaceutical education than among respondents without such education, although this difference is not statistically significant. However, depending on the education, significant differences (more than 10 %) were observed among the respondents regarding interest in the composition of vaccines, adherence to vaccination against COVID-19 of their children older than 12 years and the opening of vaccination points in pharmacies.
Conclusions. It was found that to increase the level of awareness of medical and pharmaceutical professionals regarding vaccination, it is necessary to optimize educational professional programs and curricula for their training. It is shown that increasing the level of their knowledge will increase the commitment of parents with other education to children's vaccinations. The need to expand the professional role of pharmacists by involving them in vaccinations has been confirmed
References
- Kotvitska, A. A., Kubarieva, I. V., Surikova, I. O. (2017). Determination of the content and formation of the concept of social pharmacy in the world and in Ukraine. Socìalʹna Farmacìâ v Ohoronì Zdorov’â, 3 (4), 3–9. doi: https://doi.org/10.24959/sphhcj.17.101
- Rocha, Y. M., de Moura, G. A., Desidério, G. A., de Oliveira, C. H., Lourenço, F. D., de Figueiredo Nicolete, L. D. (2021). The impact of fake news on social media and its influence on health during the COVID-19 pandemic: a systematic review. Journal of Public Health, 9. doi: https://doi.org/10.1007/s10389-021-01658-z
- Pro zakhyst naselennia vid infektsiinykh khvorob (2000). Zakon Ukrainy No. 1645-III. 06.04.2000. Available at: https://zakon.rada.gov.ua/laws/show/1645-14#Text
- Pro poriadok provedennia profilaktychnykh shcheplen v Ukraini ta kontrol yakosti y obihu medychnykh imunobiolohichnykh preparativ (2011). Nakaz MOZ Ukrainy No. 595. 16.09.2011. Available at: https://zakon.rada.gov.ua/laws/show/z1159-11#Text
- Allan, N., Harden, J. (2014). Parental decision-making in uptake of the MMR vaccination: a systematic review of qualitative literature. Journal of Public Health, 37 (4), 678–687. doi: https://doi.org/10.1093/pubmed/fdu075
- Benin, A. L., Wisler-Scher, D. J., Colson, E., Shapiro, E. D., Holmboe, E. S. (2006). Qualitative Analysis of Mothers’ Decision-Making About Vaccines for Infants: the Importance of Trust. Pediatrics, 117 (5), 1532–1541. doi: https://doi.org/10.1542/peds.2005-1728
- Gualano, M., Olivero, E., Voglino, G., Corezzi, M., Rossello, P., Vicentini, C., Bert, F., Siliquini, R. (2019). Knowledge, attitudes and beliefs towards compulsory vaccination: a systematic review. Human Vaccines & Immunotherapeutics, 15 (4), 918–931. doi: https://doi.org/10.1080/21645515.2018.1564437
- Frew, P. M., Fisher, A. K., Basket, M. M., Chung, Y., Schamel, J., Weiner, J. L. (2016). Changes in childhood immunization decisions in the United States: Results from 2012 & 2014 National Parental Surveys. Vaccine, 34 (46), 5689–5696. doi: https://doi.org/10.1016/j.vaccine.2016.08.001
- Dyda, A., King, C., Dey, A., Leask, J., Dunn, A. G. (2020). A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination. BMC Public Health, 20 (1). doi: https://doi.org/10.1186/s12889-020-09327-8
- Kundi, M., Obermeier, P., Helfert, S., Oubari, H., Fitzinger, S., Yun, J., Brix, M., Rath, B. (2015). The Impact of the Parent-Physician Relationship on Parental Vaccine Safety Perceptions. Current Drug Safety, 10 (1), 16–22. doi: https://doi.org/10.2174/157488631001150407104320
- Ramprasad, C., Zachariah, R., Steinhoff, M., Simon, A. (2016). Parental attitudes towards influenza vaccination for children in South India. World Journal of Pediatrics, 13 (1), 84–90. doi: https://doi.org/10.1007/s12519-016-0053-7
- Danchin, M. H., Costa-Pinto, J., Attwell, K., Willaby, H., Wiley, K., Hoq, M., Leask, J., Perrett, K. P., O’Keefe, J., Giles, M. L., Marshall, H. (2018). Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine, 36 (44), 6473–6479. doi: https://doi.org/10.1016/j.vaccine.2017.08.003
- Mohd Azizi, F. S., Kew, Y., Moy, F. M. (2017). Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine, 35 (22), 2955–2961. doi: https://doi.org/10.1016/j.vaccine.2017.04.010
- Costa-Pinto, J. C., Willaby, H. W., Leask, J., Hoq, M., Schuster, T., Ghazarian, A. et al. (2017). Parental Immunisation Needs and Attitudes Survey in paediatric hospital clinics and community maternal and child health centres in Melbourne, Australia. Journal of Paediatrics and Child Health, 54 (5), 522–529. doi: https://doi.org/10.1111/jpc.13790
- Grossman, Z., Hadjipanayis, A., Degani, A., Somekh, E. (2019). Tracking Changes in Vaccine Attitudes and Decisions: Results from 2008 and 2016 Parental Surveys. Pediatric Infectious Disease Journal, 38 (4), e75–e76. doi: https://doi.org/10.1097/inf.0000000000002147
- Elran, B., Yaari, S., Glazer, Y., Honovich, M., Grotto, I., Anis, E. (2018). Parents' perceptions of childhood immunization in Israel: Information and concerns. Vaccine, 36 (52), 8062–8068. doi: https://doi.org/10.1016/j.vaccine.2018.10.078
- Napolitano, F., D'Alessandro, A., Angelillo, I.F. (2018). Investigating Italian parents' vaccine hesitancy: A cross-sectional survey. Human Vaccines & Immunotherapeutics, 14 (7), 1558–1565. doi: https://doi.org/10.1080/21645515.2018.1463943
- Giannakou, K., Kyprianidou, M., Hadjikou, A., Fakonti, G., Photiou, G., Tzira, E., Heraclides, A. (2021). Knowledge of mothers regarding children’s vaccinations in Greece: an online cross-sectional study. BMC Public Health, 21 (1). doi: https://doi.org/10.1186/s12889-021-12179-5
- Sabahelzain, M. M., Moukhyer, M., Bosma, H., van den Borne, B. (2021). Determinants of Measles Vaccine Hesitancy among Sudanese Parents in Khartoum State, Sudan: A Cross-Sectional Study. Vaccines, 10 (1), 6. doi: https://doi.org/10.3390/vaccines10010006
- Skirrow, H., Barnett, S., Bell, S., Riaposova, L., Mounier-Jack, S., Kampmann, B., Holder, B. (2022). Women’s views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: a multi-methods study in the UK. BMC Pregnancy and Childbirth, 22 (1). doi: https://doi.org/10.1186/s12884-021-04321-3
- Chukhray, I. L., Antonchak, Z. P., Grushkovska, D. T. (2012). Study of parents’ attitude to the problem of compulsory immunization of children. Український медичний альманах, 15 (5), 207–208.
- Dorykevych, K. I., Kremin, Yu. I. (2021). Study of the attitude of Ukrainian citizens to vaccination: the results of an online survey. Annaly Mechnikovskoho Instytutu, 1, 51–56. doi: https://doi.org/10.5281/zenodo.6350180
- Lytras, T., Kopsachilis, F., Mouratidou, E., Papamichail, D., Bonovas, S. (2015). Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Human Vaccines & Immunotherapeutics, 12 (3), 671–681. doi: https://doi.org/10.1080/21645515.2015.1106656
- Report of the SAGE working group on vaccine hesitancy (2014). The Strategic Advisory Group of Experts (SAGE). World Health Organization.
- Tafuri, S. S., Martinelli, D. D., Caputi, G. G., Arbore, A. A., Germinario, C. C., Prato, R. R. (2009). Italian healthcare workers’ views on mandatory vaccination. BMC Health Services Research, 9 (1). doi: https://doi.org/10.1186/1472-6963-9-100
- Martinelli, D., Tafuri, S., Fortunato, F., Cozza, V., Germinario, C. A., Prato, R. (2014). Are we ready to abrogate compulsory vaccinations for children? Human Vaccines & Immunotherapeutics, 11 (1), 146–149. doi: https://doi.org/10.4161/hv.34417
- Nicolay, N., Lévy-Bruhl, D., Gautier, A., Jestin, C., Jauffret-Roustide, M. (2008). Mandatory immunization: The point of view of the French general population and practitioners. Vaccine, 26 (43), 5484–5493. doi: https://doi.org/10.1016/j.vaccine.2008.07.058
- Fedyak, I. O., Bilyk, I. P., Mateyko, G. B. (2018). Focus on vaccination: the view of doctors and analysis of its pharmaceutical support on children’s bacterial infections. Pharmaceutical Review, 1, 139–151. doi: https://doi.org/10.11603/2312-0967.2018.1.8698
- Vaktsynatsiia: pytannia ta vidpovidi (Pryvyvky – vaktsyny – shcheplennia). Available at: https://www.facebook.com/groups/bzvorgua/permalink/1577574825771355/4
- «Vaktsynatsyia protyv zdorovia! Mi za svobodu vibora! (Ukrayna)». Available at: https://www.facebook.com/groups/811537635696912/
- Yashkina, O. I. (2013). Statistical tools of expert opinion consistency in marketing research. Ekonomichnyi visnyk Natsionalnoho tekhnichnoho universytetu Ukrainy "Kyivskyi politekhnichnyi instytut", 10, 442–449. Available at: http://nbuv.gov.ua/UJRN/evntukpi_2013_10_74
- Derzhavna sluzhba statystyky Ukrainy. Available at: http://ukrstat.gov.ua/
- Hromovyk, B. P., Korolyov, M. V. (2020). The results of the study of pharmacists’ opinion regarding the organization of their work in pharmacies during the coronavirus COVID-19 pandemic. Farmatsevtychnyi Zhurnal, 3, 39–44. doi: https://doi.org/10.32352/0367-3057.3.20.04
- Moskalenko, V. F. (Ed.) (2009). Biostatystyka. Kyiv: Knyha plius, 184.
- Pro vvedennia v diiu Rishennia operatyvnoho shtabu Ministerstva okhorony zdorovia Ukrainy z reahuvannia na sytuatsii z poshyrennia infektsiinykh khvorob, yakym mozhna zapobihty shliakhom vaktsynatsii vid 01 zhovtnia 2021 roku (2021). Nakaz MOZ Ukrainy No. 2234. 13.10.2021. Available at: https://cutt.ly/WGvznpX
- V Ukraini rozpochynaietsia pilotnyi proiekt iz vaktsynatsii proty hrypu v aptekakh. Available at: https://moz.gov.ua/article/news/v-ukraini-rozpochinaetsja-pilotnij-proekt-iz-vakcinacii-proti-gripu-v-aptekah
- Demchenko, I., Kozhan, N., Holtsas, L., Fenchak, A. (2017). Faktory vplyvu na prykhylnist batkiv shchodo vaktsynatsii: rezultaty doslidzhennia. ATs "Sotsiokonsaltynh", 16.
- Drutsul-Melnyk, N. V., Ivanova, L. A., Koloskova, O. K., Haras, M. N. (2022). Do pytannia imunoprofilaktyky infektsiinykh khvorob u ditei v period pandemii SOVID-19. Visnyk medychnykh i biolohichnykh doslidzhen, 2, 24–29. doi: https://doi.org/10.11603/bmbr.2706-6290.2022.2.13045
- Rhodes, L. A., Williams, D. M., Marciniak, M. W., Weber, D. J. (2017). Community pharmacists as vaccine providers. International Journal of Health Governance, 22 (3), 167–182. doi: https://doi.org/10.1108/ijhg-05-2017-0020
- Isenor, J. E., Edwards, N. T., Alia, T. A., Slayter, K. L., MacDougall, D. M., McNeil, S. A., Bowles, S. K. (2016). Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis. Vaccine, 34 (47), 5708–5723. doi: https://doi.org/10.1016/j.vaccine.2016.08.085
- Le, L. M., Veettil, S. K., Donaldson, D., Kategeaw, W., Hutubessy, R., Lambach, P., Chaiyakunapruk, N. (2022). The impact of pharmacist involvement on immunization uptake and other outcomes: An updated systematic review and meta-analysis. Journal of the American Pharmacists Association, 62 (5), 1499–1513.e16. doi: https://doi.org/10.1016/j.japh.2022.06.008
- Poliakova, D. (2020). Shcheplennia v aptetsi: yevropeiski modeli ta dosvid. Apteka.ua online, 29 (1250). Available at: https://www.apteka.ua/article/553207
- The legal and regulatory framework for community pharmacies in the WHO European Region (2019). Copenhagen: WHO. Available at: https://apps.who.int/iris/bitstream/handle/10665/326394/9789289054249-eng.pdf?sequence=1&isAllowed=y
- Pinto, G. S., Hung, M., Wong, A. (2020). An overview of pharmacy's impact on immunization coverage. A global survey 2020. International Pharmaceutical Federation (FIP). The Hague: International Pharmaceutical Federation, 66. Available at: https://www.fip.org/file/4751
- Isler, A. (2022). Can Kids Under 5 Get the COVID Vaccine at a Pharmacy? Available at: https://www.verywellhealth.com/young-children-covid-vaccine-pharmacy-or-pediatrician-5496841
- Omecene, N. E., Patterson, J. A., Bucheit, J. D., Anderson, A. N., Rogers, D., Goode, J.-V. R., Caldas, L. M. (2019). Pharmacist-administered pediatric vaccination services in the United States: major barriers and potential solutions for the outpatient setting. Pharmacy Practice, 17 (2), 1581. doi: https://doi.org/10.18549/pharmpract.2019.2.1581
- Hanretty, A., Rose L. (2020). New HHS Regulations Expand Pharmacists’ Role in Childhood Immunizations. Pharmacy times. Available at: https://www.pharmacytimes.com/view/new-hhs-regulations-expand-pharmacists-role-in-childhood-immunizations
- PREP Act immunity from liability for COVID-19 vaccinators (2019). Department of Health and Human Services. Available at: https://www.phe.gov/emergency/events/COVID19/COVIDVaccinators/Pages/PREP-Act-Immunity-from-Liability-for-COVID-19-Vaccinators.aspx
- Pharmacist administered vaccines: based on NASPA analysis of state pharmacy practice laws (2022). American Pharmacists Association; National Alliance of State Pharmacy Associations. Available at: https://naspa.us/wp-content/uploads/2022/06/Pharmacist-Immunization-Authority-June-2022.pdf
- American Academy of Pediatrics Opposes HHS Action on Childhood Vaccines; Calls It ‘Incredibly Misguided’. (2020). American Academy of Pediatrics. Available at: https://www.aap.org/en/news-room/news-releases/aap/2020/american-academy-of-pediatrics-opposes-hhs-action-on-childhood-vaccines-calls-it-incredibly-misguided/
- Zaprutko, T., Kremin, Y., Michalak, M., Bernatoniene, J., Zaprutko, L., Hudz, N. et al. (2022). Social Attitude to COVID-19 and Influenza Vaccinations after the Influenza Vaccination Season and between the Second and Third COVID-19 Wave in Poland, Lithuania, and Ukraine. International Journal of Environmental Research and Public Health, 19 (4), 2042. doi: https://doi.org/10.3390/ijerph19042042
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Iryna Chukhray, Oksana Levytska, Рetro Oliinyk, Iryna Hadiak, Halyna Bilushchak

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.






