The pharmacotherapy management of cardiovascular diseases in hospitalised patients: clinical pharmacist’s view
DOI:
https://doi.org/10.15587/2519-4852.2024.303427Keywords:
management, cardiovascular diseases, inpatients, drugs enhancing the cardiac metabolism, drug-related problemsAbstract
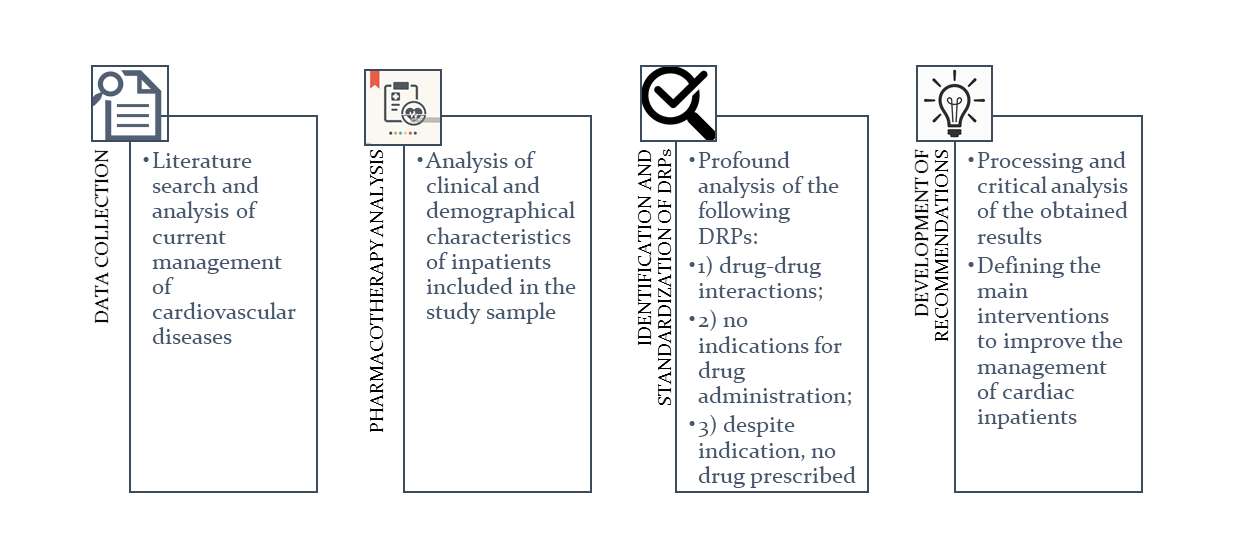
The aim. To assess pharmacotherapy of hospitalised patients with coronary heart disease in Ukraine, identify the types of drug-related problems, and recommend interventions to improve the management of cardiac inpatients.
Materials and methods. The objects of the study were 25 medical records of inpatients with coronary heart disease complicated by heart failure and atherosclerotic cardiosclerosis. Methods applied: systematisation, generalisation, comparison, clinical and pharmaceutical approach. The statistical analyses were performed using the SPSS Trial.
Results. A comprehensive retrospective study was conducted to assess the management of cardiovascular diseases. In total, 25 patients were prescribed 62 drugs. It was established that 53.5 % of medicines were "Agents affecting the cardiovascular system"; out of them, 26.9 % were "other cardiac drugs" (C01E) used for enhancing cardiac energy metabolism. The study identified 597 drug-related problems (DRPs) (23.9±12.6 DRPs per patient) with the drug-drug interactions prevalence (62.6 %). Other common groups of DRPs were: (1) no indications for drug administration (8.5 %), and (2) despite indications, the drug was not prescribed (8.2 %). 99 DRPs (16.6 %; 95 % CI:13.7-19.8 %) were associated with "other cardiac drugs". They included 4 types of DRPs: (1) no indications for drug administration (33.3 %); (2) insufficient duration of the treatment (31.3 %); (3) drug-drug interactions (22.3 %); and (4) insufficient dosage or frequency of use (13.1 %).
Conclusion. Our findings suggest that the treatment of cardiac inpatients is associated with numerous DRPs. Thus, we formed a list of recommendations to improve the management of cardiovascular diseases in hospitalised patients
References
- Cardiovascular disease the world’s number 1 killer (2021). World Heart Federation. Available at: https://world-heart-federation.org/wp-content/uploads/2021/07/WHF-CVD-Number-1-Killer-2021.pdf
- Davidson, K. W., Barry, M. J., Mangione, C. M., Cabana, M., Chelmow, D., Coker, T. R. et al. (2022). Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement. JAMA, 327 (16), 1577–1584. https://doi.org/10.1001/jama.2022.4983
- Sertsevo-sudynni zakhvoriuvannia – holovna prychyna smerti ukraintsiv. Vysnovky z doslidzhennia hlobalnoho tiaharia khvorob u 2019 rotsi (2021). Tsentr hromadskoho zdorovia Ministerstva okhorony zdorovia Ukrainy. Available at: https://phc.org.ua/news/sercevo-sudinni-zakhvoryuvannya-golovna-prichina-smerti-ukrainciv-visnovki-z-doslidzhennya.
- STEPS: prevalence of noncommunicable disease risk factors in Ukraine 2019 (2020). Copenhagen: WHO Regional Office for Europe. Available at: https://ukraine.un.org/sites/default/files/2020-11/WHO-EURO-2020-1468-41218-56060-eng_0.pdf
- Sirenko, Yu. M. (2022). The state of the problem of cardiovascular morbidity and mortality in Ukraine. Medicine of Ukraine, 2 (258), 11–14. https://doi.org/10.37987/1997-9894.2022.2(258).264084
- Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019 (2020). Geneva: World Health Organization. Available at: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death
- Visseren, F. L. J., Mach, F., Smulders, Y. M., Carballo, D., Koskinas, K. C., Bäck, M. et al. (2021). 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal, 42 (34), 3227–3337. https://doi.org/10.1093/eurheartj/ehab484
- Arnett, D. K., Blumenthal, R. S., Albert, M. A., Buroker, A. B., Goldberger, Z. D., Hahn, E. J. et al. (2019). 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 140 (11), e563–e595. https://doi.org/10.1161/cir.0000000000000677
- Regmi, M., Siccardi, M. A. (2023). Coronary Artery Disease Prevention. StatPearls. StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK547760/
- Stabilna ishemichna khvoroba sertsia klinichna nastanova, zasnovana na dokazakh (2021). Derzhavnyi ekspertnyi tsentr Ministerstva okhorony zdorovia Ukrainy, 148. Available at: https://www.dec.gov.ua/wp-content/uploads/2021/12/2021_10_26_kn_stabilna-ihs.pdf
- Knuuti, J., Wijns, W., Saraste, A., Capodanno, D., Barbato, E., Funck-Brentano, C. et al. (2019). 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal, 41 (3), 407–477. https://doi.org/10.1093/eurheartj/ehz425
- V. Tran, A., T. Nguyen, D., K. Tran, S., H. Vo, T., T. Nguyen, K., M. Nguyen, P. et al. (2022). Drug-Related Problems in Coronary Artery Diseases. Coronary Artery Bypass Grafting. IntechOpen. https://doi.org/10.5772/intechopen.103782
- Ryvak, T., Makukh, Kr., Zimenkovsky, A., Gorodnycha, O. (2014). Pharmacotherapy assessment with reference to existing cardiological practice in Ukraine. Pharmacia, 61 (1), 3–11.
- Derzhavnyi reiestr likarskykh zasobiv Ukrainy. Available at: http://www.drlz.com.ua/ibp/ddsite.nsf/all/shlist?opendocument
- Reiestr medyko-tekhnolohichnykh dokumentiv (2019). Derzhavnyi ekspertnyi tsentr MOZ Ukrainy. Available at: https://www.dec.gov.ua/mtd/home/
- Drug Interaction Checker. Medscape. Available at: https://reference.medscape.com/drug-interactionchecker
- Drug Interaction Checker. Drugs.com. Available at: https://www.drugs.com/drug_interactions.html
- Redzuan, A. M., Ramli, A. R., Pheng, M. T. H. (2017). Drug-related problems in hypertensive patients with multiple comorbidities. Journal of Pharmaceutical Research, 1 (3), 000113.
- Unifikovanyi klinichnyi protokol pervynnoi, vtorynnoi (spetsializovanoi) ta tretynnoi (vysokospetsializovanoi) medychnoi dopomohy «Stabilna ishemichna khvoroba sertsia» (2021). Nakaz Ministerstva okhorony zdorovia Ukrainy No. 2857. 23.12.2021, 58. Available at: https://www.dec.gov.ua/wp-content/uploads/2021/12/2021_2857_ykpmd_stabihs.pdf
- Valgimigli, M., Bueno, H., Byrne, R. A., Collet, J.-P., Costa, F., Jeppsson, A. et al. (2017). 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. European Heart Journal, 39 (3), 213–260. https://doi.org/10.1093/eurheartj/ehx419
- Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, D. E., Colvin, M. M. et al. (2017). 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation, 136 (6), e137–e161. https://doi.org/10.1161/cir.0000000000000509
- Villanueva, C., Albillos, A., Genescà, J., Garcia-Pagan, J. C., Calleja, J. L., Aracil, C. et al. (2019). β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet, 393 (10181), 1597–1608. https://doi.org/10.1016/s0140-6736(18)31875-0
- Niriayo, Y. L., Kifle, R., Asgedom, S. W., Gidey, K. (2024). Drug therapy problems among hospitalized patients with cardiovascular disease. BMC Cardiovascular Disorders, 24 (1). https://doi.org/10.1186/s12872-024-03710-8
- Sefera, B., Getachew, M., Babu, Y., Bekele, F., Fanta, K. (2022). Drug-related problems and its predictors among hospitalized heart failure patients at Jimma Medical Center, South West Ethiopia: prospective interventional study. BMC Cardiovascular Disorders, 22 (1). https://doi.org/10.1186/s12872-022-02859-4
- Georgiev, K. D., Hvarchanova, N., Georgieva, M., Kanazirev, B. (2019). The role of the clinical pharmacist in the prevention of potential drug interactions in geriatric heart failure patients. International Journal of Clinical Pharmacy, 41 (6), 1555–1561. https://doi.org/10.1007/s11096-019-00918-z
- Niriayo, Y. L., Kumela, K., Kassa, T. D., Angamo, M. T. (2018). Drug therapy problems and contributing factors in the management of heart failure patients in Jimma University Specialized Hospital, Southwest Ethiopia. PLOS ONE, 13(10), e0206120. https://doi.org/10.1371/journal.pone.0206120
- Seid, E., Engidawork, E., Alebachew, M., Mekonnen, D., Berha, A. B. (2020). Evaluation of drug therapy problems, medication adherence and treatment satisfaction among heart failure patients on follow-up at a tertiary care hospital in Ethiopia. PLOS ONE, 15 (8), e0237781. https://doi.org/10.1371/journal.pone.0237781
- Wsół, A., Mamcarz, A. (2016). Miejsce leczenia metabolicznego stabilnej choroby wieńcowej: teraźniejszość i perspektywy. Przegląd Lekarski, 73 (6), 395–398.
- Heggermont, W. A., Papageorgiou, A., Heymans, S., van Bilsen, M. (2016). Metabolic support for the heart: complementary therapy for heart failure? European Journal of Heart Failure, 18 (12), 1420–1429. https://doi.org/10.1002/ejhf.678
- Chrusciel, P., Rysz, J., Banach, M. (2014). Defining the Role of Trimetazidine in the Treatment of Cardiovascular Disorders: Some Insights on Its Role in Heart Failure and Peripheral Artery Disease. Drugs, 74 (9), 971–980. https://doi.org/10.1007/s40265-014-0233-5
- Marzilli, M., Vinereanu, D., Lopaschuk, G., Chen, Y., Dalal, J. J., Danchin, N. et al. (2019). Trimetazidine in cardiovascular medicine. International Journal of Cardiology, 293, 39–44. https://doi.org/10.1016/j.ijcard.2019.05.063
- Shu, H., Peng, Y., Hang, W., Zhou, N., Wang, D. W. (2021). Trimetazidine in Heart Failure. Frontiers in Pharmacology, 11. https://doi.org/10.3389/fphar.2020.569132
- Truong, T. T. A., Phan, N. K., Vo, Q. V., Diep, H. G., Vuong, H. T. K., Le, T. V. et al. (2019). Drug‐related problems in prescribing for coronary artery diseases in Vietnam: cross‐sectional study. Tropical Medicine & International Health, 24 (11), 1335–1340. https://doi.org/10.1111/tmi.13310
- Amankwa Harrison, M., Marfo, A. F. A., Buabeng, K. O., Nkansah, F. A., Boateng, D. P., Ankrah, D. N. A. (2022). Drug‐related problems among hospitalized hypertensive and heart failure patients and physician acceptance of pharmacists’ interventions at a teaching hospital in Ghana. Health Science Reports, 5 (5). https://doi.org/10.1002/hsr2.786
- Ciapponi, A., Fernandez Nievas, S. E., Seijo, M., Rodríguez, M. B., Vietto, V., García-Perdomo, H. A. et al. (2021). Reducing medication errors for adults in hospital settings. Cochrane Database of Systematic Reviews, 2021 (11). https://doi.org/10.1002/14651858.cd009985.pub2
- Savarese, G., Lund, L. H. (2017). Global Public Health Burden of Heart Failure. Cardiac Failure Review, 3 (1), 7–11. https://doi.org/10.15420/cfr.2016:25:2
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Tetiana Ryvak, Oksana Horodnycha

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.






