Current state of scientific research on pharmacological correction of mammary gland pathologies (a scoping review)
DOI:
https://doi.org/10.15587/2519-4852.2025.348372Keywords:
mammary gland pathologies, pharmacological correction, method analysis, scoping reviewAbstract
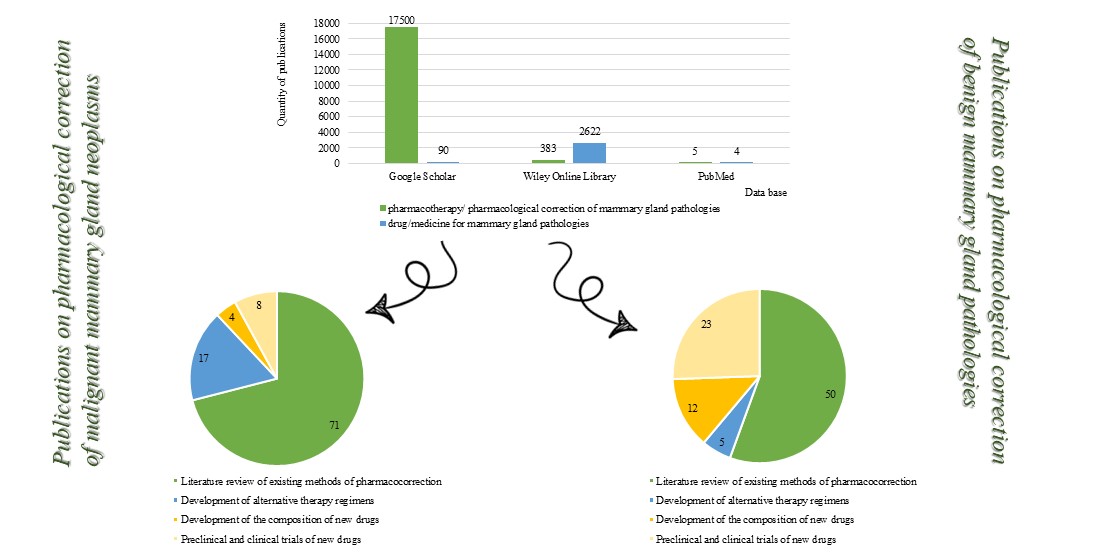
The aim of the study is to conduct a bibliosemantic analysis of scientific literature on pharmacological correction of breast pathologies and to determine the proportion of studies on pharmacological correction of mastopathy.
Materials and methods. In the context of our study, the analysis of data on the current state of research on the pharmacological correction of mammary gland pathologies and the identification of the proportion of studies focusing on the pharmacological correction of mastopathy was carried out using the enhanced Arksey & O’Malley methodology proposed by a group of researchers led by H.M. Daudt. A total of 540 publications (from the last five years) were reviewed.
Results. The results of the study showed that the vast majority of publications are devoted to the pharmacological correction of breast cancer (78%). Studies on the pharmacological correction of mastopathy make up a significantly smaller share (22%), which confirms their relevance, particularly regarding the development of original drugs. Among these, herbal-based medicinal products are most commonly used as part of combination therapy (59%).
Conclusions. Studying the current state of scientific research on a given topic is an integral part of planning and developing a strategy for one's own research. A detailed analysis of the available literature makes it possible to identify unresolved issues that remain unaddressed by researchers from different countries, and to outline relevant niches for further scientific investigation.
A bibliosemantic analysis of scientific literature on pharmacological correction of breast pathologies was conducted, and the relevance of conducting research on the development of herbal remedies for the pharmacological correction of mastopathy was established.
References
- Dhari, Z. A., Sultan, A. H., Shubber, L. A., Al_Ameri, Hiba. D. (2022). Association between polycystic ovary and fibrocystic breast by ultrasound. International Journal of Health Sciences, 6 (2), 11420–11428. https://doi.org/10.53730/ijhs.v6ns2.7435
- Paik, S., Murthy, B. (2025). Effectiveness of mammography and ultrasound in differentiating fibroadenomas from other benign breast lesions in the context of fibrocystic changes. International Journal for Multidisciplinary Research, 7(5): 1–5. https://doi.org/10.36948/ijfmr.2025.v07i05.557
- Faguy, K. (2022). Fibrocystic Breast Changes. Radiologic technology, 93 (3), 303M–315M.
- Lunko, T. A., Lytvynenko, O. O., Lunko, A. S., Konovalenko, S. V., Khmel, A. V. (2025). Breast cancer is a threatening scenario resulting from the development of endometriosis and benign breast disease overlap syndrome: literature review. International Journal of Endocrinology, 21 (2), 206–214. https://doi.org/10.22141/2224-0721.21.2.2025.1520
- Bhagat, S., Ekka, R., Ahirwar, B. (2025). A Comprehensive data to Understanding the Molecular Mechanism Involving Breast Cancer. Research Journal of Pharmacy and Technology, 18 (7), 3374–3384. https://doi.org/10.52711/0974-360x.2025.00488
- Expert consensus on the clinical application of PI3K/AKT/mTOR inhibitors in the treatment of advanced breast cancer (2022). Cancer Innovation, 1 (1), 25–54. https://doi.org/10.1002/cai2.10
- Bradley, R., Braybrooke, J., Gray, R., Hills, R. K., Liu, Z., Pan, H. et al. (2022). Aromatase inhibitors versus tamoxifen in premenopausal women with oestrogen receptor-positive early-stage breast cancer treated with ovarian suppression: a patient-level meta-analysis of 7030 women from four randomised trials. The Lancet Oncology, 23 (3), 382–392. https://doi.org/10.1016/s1470-2045(21)00758-0
- Peng, Y., Binghe, X. (2022). Expert consensus on off-label use of small molecule anti-angiogenic drugs in the treatment of metastatic breast cancer. Chinese journal of oncology, 44 (6), 523–530. https://doi.org/10.3760/cma.j.cn112152-20220310-00168
- Sydora, N., Konovalova, O., Zuikina, S., Semchenko, K., Rudnyk, A., Hurtovenko, I. (2021). Comparative study the essential oil composition of flowers and leaves of Crataegus monogyna L. ScienceRise: Pharmaceutical Science, 6 (34), 20–26. https://doi.org/10.15587/2519-4852.2021.249276
- Sydora, N., Yakovenko, V., Ochkur, O., Rudnyk, A., Honcharov, O., Zuikina, S. et al. (2023). Technology of obtaining and chemical profiles of dry extracts from leaves of prospective species of the hawthorn genus. ScienceRise: Pharmaceutical Science, 1 (41), 58–66. https://doi.org/10.15587/2519-4852.2023.274772
- Matsiuk, K., Kovalova, T., Maslii, Y., Herbina, N., Vyshnevska, L., Kaliuzhnaia, O., Tkachuk, O. (2023). Experimental research on the development of composition of complex action ointment based on phytocomplex. ScienceRise: Pharmaceutical Science, 4 (44), 19–27. https://doi.org/10.15587/2519-4852.2023.286306
- Vyshnevska, L., Khokhlova, K., Yakovenko, V., Postoy, V. (2021). Study on Identification of Active Ingredients of Combined Gel with Salvia and Willow Plant Extracts. Pharmacology OnLine, 1, 130–135. Available at: https://dspace.nuph.edu.ua/handle/123456789/27200
- Shmalko, O., Kovalova, T., Bodnar, L., Kovalov, V., Yakovenko, V., Vyshnevska, L. (2024). Development of an emulsion composition with fennel and caraway essential oils for use in the combined therapy of ulcerative colitis. ScienceRise: Pharmaceutical Science, 2 (48), 74–82. https://doi.org/10.15587/2519-4852.2024.302941
- Shukla, P., Misra, P., Jain, R. K., Misra, R. K. (2022). Homoeopathic Treatment of Fibrocystic Breast Diseases: A Case Series. Homœopathic Links, 35 (1), 62–69. https://doi.org/10.1055/s-0041-1741462
- Daudt, H. M., van Mossel, C., Scott, S. J. (2013). Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology, 13 (1). https://doi.org/10.1186/1471-2288-13-48
- Trayes, K. P., Cokenakes, S. E. H. (2021) Breast Cancer Treatment. American family physician, 104 (2), 171–178. https://pubmed.ncbi.nlm.nih.gov/34383430/
- Kerr, A. J., Dodwell, D., McGale, P., Holt, F., Duane, F., Mannu, G., Darby, S. C., Taylor, C. W. (2022). Adjuvant and neoadjuvant breast cancer treatments: A systematic review of their effects on mortality. Cancer Treatment Reviews, 105, 102375. https://doi.org/10.1016/j.ctrv.2022.102375
- Barzaman, K., Karami, J., Zarei, Z., Hosseinzadeh, A., Kazemi, M. H., Moradi-Kalbolandi, S. et al. (2020). Breast cancer: Biology, biomarkers, and treatments. International Immunopharmacology, 84, 106535. https://doi.org/10.1016/j.intimp.2020.106535
- Ben-Dror, J., Shalamov, M., Sonnenblick, A. (2022). The History of Early Breast Cancer Treatment. Genes, 13 (6), 960. https://doi.org/10.3390/genes13060960
- Desai, P., Aggarwal, A. (2021). Breast Cancer in Women Over 65 years- a Review of Screening and Treatment Options. Clinics in Geriatric Medicine, 37 (4), 611–623. https://doi.org/10.1016/j.cger.2021.05.007
- Sarhangi, N., Hajjari, S., Heydari, S. F., Ganjizadeh, M., Rouhollah, F., Hasanzad, M. (2022). Breast cancer in the era of precision medicine. Molecular Biology Reports, 49 (10), 10023–10037. https://doi.org/10.1007/s11033-022-07571-2
- Xiong, X., Zheng, L.-W., Ding, Y., Chen, Y.-F., Cai, Y.-W., Wang, L.-P. et al. (2025). Breast cancer: pathogenesis and treatments. Signal Transduction and Targeted Therapy, 10 (1). https://doi.org/10.1038/s41392-024-02108-4
- Dastjerd, N. T., Valibeik, A., Rahimi Monfared, S., Goodarzi, G., Moradi Sarabi, M., Hajabdollahi, F. et al. (2022). Gene therapy: A promising approach for breast cancer treatment. Cell Biochemistry and Function, 40 (1), 28–48. https://doi.org/10.1002/cbf.3676
- Cavalcante, F. P., Millen, E. C., Zerwes, F. P., Novita, G. G. (2020). Progress in Local Treatment of Breast Cancer: A Narrative Review. Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics, 42 (6), 356–364. https://doi.org/10.1055/s-0040-1712125
- Dvir, K., Giordano, S., Leone, J. P. (2024). Immunotherapy in Breast Cancer. International Journal of Molecular Sciences, 25 (14), 7517. https://doi.org/10.3390/ijms25147517
- Jacobs, A. T., Martinez Castaneda-Cruz, D., Rose, M. M., Connelly, L. (2022). Targeted therapy for breast cancer: An overview of drug classes and outcomes. Biochemical Pharmacology, 204, 115209. https://doi.org/10.1016/j.bcp.2022.115209
- Bourang, S., Noruzpour, M., Jahanbakhsh Godekahriz, S., Ebrahimi, H. A. C., Amani, A., Asghari Zakaria, R., Yaghoubi, H. (2024). Application of nanoparticles in breast cancer treatment: a systematic review. Naunyn-Schmiedeberg’s Archives of Pharmacology, 397 (9), 6459–6505. https://doi.org/10.1007/s00210-024-03082-y
- Dai, Y., Liang, P., Yu, J. (2022). Percutaneous Management of Breast Cancer: a Systematic Review. Current Oncology Reports, 24 (11), 1443–1459. https://doi.org/10.1007/s11912-022-01290-4
- Rodin, D., Glicksman, R. M., Hepel, J. T., Huber, K., Kirova, Y., Loap, P., Rakovitch, E. (2024). Early-Stage Breast Cancer: A Critical Review of Current and Emerging Practice. International Journal of Radiation Oncology, Biology, Physics, 120 (5), 1260–1272. https://doi.org/10.1016/j.ijrobp.2024.08.037
- Upadhyay, R., Bazan, J. G. (2023). Advances in Radiotherapy for Breast Cancer. Surgical Oncology Clinics of North America, 32 (3), 515–536. https://doi.org/10.1016/j.soc.2023.03.002
- Vieira, C., Piperis, M. N., Sagkriotis, A., Cottu, P. (2022). Systemic treatment for hormone receptor-positive/HER2-negative advanced/metastatic breast cancer: A review of European real-world evidence studies. Critical Reviews in Oncology/Hematology, 180, 103866. https://doi.org/10.1016/j.critrevonc.2022.103866
- Kunde, S. S., Wairkar, S. (2022). Targeted delivery of albumin nanoparticles for breast cancer: A review. Colloids and Surfaces B: Biointerfaces, 213, 112422. https://doi.org/10.1016/j.colsurfb.2022.112422
- Ye, F., Dewanjee, S., Li, Y., Jha, N. K., Chen, Z.-S., Kumar, A. et al. (2023). Advancements in clinical aspects of targeted therapy and immunotherapy in breast cancer. Molecular Cancer, 22 (1). https://doi.org/10.1186/s12943-023-01805-y
- Costa, A., Vale, N. (2021). Strategies for the treatment of breast cancer: from classical drugs to mathematical models. Mathematical Biosciences and Engineering, 18 (5), 6328–6385. https://doi.org/10.3934/mbe.2021316
- Wang, Y., Minden, A. (2022). Current Molecular Combination Therapies Used for the Treatment of Breast Cancer. International Journal of Molecular Sciences, 23 (19), 11046. https://doi.org/10.3390/ijms231911046
- Gheysen, M., Punie, K., Wildiers, H., Neven, P. (2024). Oral SERDs changing the scenery in hormone receptor positive breast cancer, a comprehensive review. Cancer Treatment Reviews, 130, 102825. https://doi.org/10.1016/j.ctrv.2024.102825
- Duso, B. A., Trapani, D., Marra, A., D’Amico, P., Guerini Rocco, E., Fusco, N. et al. (2020). Pharmacological management of male breast cancer. Expert Opinion on Pharmacotherapy, 21 (12), 1493–1504. https://doi.org/10.1080/14656566.2020.1763305
- Lalagkas, P. N., Melamed, R. D. (2024). Shared genetics between breast cancer and predisposing diseases identifies novel breast cancer treatment candidates. Human Genomics, 18 (1). https://doi.org/10.1186/s40246-024-00688-4
- Gautam, S., Jindal, P., Joshi, S., Maurya, R., Patel, P., Gupta, G. D., Kurmi, B. D. (2026). Recent Developments in Vesicular Nanocarriers for Targeted Drug Delivery in Breast Cancer. Current Pharmaceutical Design, 32 (7), 519–533. https://doi.org/10.2174/0113816128385024250625212516
- Dos Reis, C. C., Marcolongo-Pereira, C., Quintela-Castro, F. C. de A., Rossoni Junior, J. V., Barcelos, R. M., Fernandes Teixeira, S. (2025). Drug interaction in breast cancer patients. UNESC Em Revista, 9 (1), 63–81. https://doi.org/10.54578/unesc.v9i1.494
- Basin, B. (2023). New Drugs for Breast Cancer Treatment. Texila International Journal Of Academic Research, 10 (3), 26–33. https://doi.org/10.21522/tijar.2014.10.03.art003
- Tang, X. (2025). Study of nanoformulations for breast cancer treatment. BIO Web of Conferences, 174, 02001. https://doi.org/10.1051/bioconf/202517402001
- Addissouky, T. A., El Sayed, I. E. T., Ali, M. M. A., Alubiady, M. H. S., Wang, Y. (2024). Harnessing innovation for the future of breast cancer management. Clinical Research in Oncology, 1 (1), 10–17. https://doi.org/10.46439/oncology.1.004
- Kong, Z., Ren, B., Liu, F., Lan, M., Li, L., Zou, T. et al. (2024). Adipocyte: an assistant to breast cancer development and a potential treatment strategy for breast cancer. Authorea. https://doi.org/10.22541/au.170668559.94144459/v1
- Basharat, S. I., Conteh, C. K., Jamil, M.; Zaman, M. A., Farooqi, S. H., Khan, A. M. A. (Eds.) (2025). Drug resistance in breast cancer and nanotherapeutical advancements. Holistic Health and Antimicrobial Resistance: A Zoonotic Perspective. Faisalabad: Unique Scientific Publishers, 162–168. https://doi.org/10.47278/book.HH/2025.48
- Sharifi-Ardani, S. E., Fathollahzadeh, M., Ghazizadeh, Y., Tajik, N., Hosseinabadi, T. (2024). Nanocarriers for curcumin in breast cancer therapy: A review. 24th Iranian Pharmacy Students’ Seminar. Tehran.
- Agarwal, V., Mahajan, M. U., Singh, R. (2024). Antibody-drug conjugate review in breast cancer: A targeted approach. International Journal of Molecular and Immuno Oncology, 9, 104–110. https://doi.org/10.25259/ijmio_30_2024
- Davis, A. A., Hesse, J., Pereira, P. M. R., Ma, C. X. (2025). Novel treatment approaches utilizing antibody-drug conjugates in breast cancer. Npj Breast Cancer, 11(1). https://doi.org/10.1038/s41523-025-00743-w
- Saha, B., Gautam, D. (2025). Targeted Therapy for Breast Cancer Treatment. International Journal of Innovative Science and Research Technology, 10 (4), 211–216. https://doi.org/10.38124/ijisrt/25apr129
- Shao, H., Varamini, P. (2022). Breast Cancer Bone Metastasis: A Narrative Review of Emerging Targeted Drug Delivery Systems. Cells, 11 (3), 388. https://doi.org/10.3390/cells11030388
- Ashrafizadeh, M., Zarrabi, A., Bigham, A., Taheriazam, A., Saghari, Y., Mirzaei, S. et al. (2023). (Nano)platforms in breast cancer therapy: Drug/gene delivery, advanced nanocarriers and immunotherapy. Medicinal Research Reviews, 43 (6), 2115–2176. https://doi.org/10.1002/med.21971
- Shirley, M. (2024). Capivasertib: First Approval. Drugs, 84 (3), 337–346. https://doi.org/10.1007/s40265-024-01998-6
- Segovia-Mendoza, M., García-Quiroz, J., Díaz, L., García-Becerra, R. (2021). Combinations of Calcitriol with Anticancer Treatments for Breast Cancer: An Update. International Journal of Molecular Sciences, 22 (23), 12741. https://doi.org/10.3390/ijms222312741
- Song, Y., Ke, X., Chen, L. (2021). The Potential Use of RNA-based Therapeutics for Breast Cancer Treatment. Current Medicinal Chemistry, 28 (25), 5110–5136. https://doi.org/10.2174/0929867327666201117100336
- Arvindekar, A., Arvindekar, S., Mali, S. N., Mali, S. (2024). Unveiling promising bioactives for breast cancer: a novel approach for herbal-based drug discovery. Phytochemistry Reviews, 24 (4), 3221–3264. https://doi.org/10.1007/s11101-024-10024-2
- Siddiqui, B., Anthony, V., Pathak, K., Singh, S., Chandrakar, R., Jain, D. (2022). Review on herbal drugs nanonization for the treatment of breast cancer. Biological Sciences, 2 (3), 291–301. https://doi.org/10.55006/biolsciences.2022.2302
- Sharma, D., Mishra, S., Rajput, A., Raj, K., Malviya, R. (2021). Pathophysiology and Biomarkers for Breast Cancer: Management Using Herbal Medicines. Current Nutrition & Food Science, 17 (9), 974–984. https://doi.org/10.2174/1573401317666210713114216
- Nishal, S., Kumar, V., Phaugat, P., Kumar, D., Khatri, N., Singh, G. (2025). A Systematic Review and Meta-Analysis of the Metal Nano-Particles Loaded with Herbal Drugs Moieties Against Breast Cancer. Recent Patents on Nanotechnology, 19 (1), 120–130. https://doi.org/10.2174/1872210518666230907115056
- Kellik Setiawan, V., Affan Ali Murtadlo, A., Nur Muhammad Ansori, A., Dhea Kharisma, V., Dayu Rahma Turista, D. (2025). The potential of Dayak tribal herbal leaves as an anti-breast cancer agent: In silico approach. BIO Web of Conferences, 153, 01006. https://doi.org/10.1051/bioconf/202515301006
- Dam, S.-M., Lam, K.-K., Le, A. D.; Rezaei, N. (Ed.) (2023). Herbal Medicine as a Complementary Therapy to Traditional Treatment for Breast Cancer. Challenges in Solid Tumors and Other Cancers: An Interdisciplinary Approach. Cham: Springer, 387–409. https://doi.org/10.1007/16833_2023_170
- Saha, S., D’souza, D., Londhe, V. Y. (2021). Exploring the concepts of various nano-formulations loaded with herbal drugs moieties against breast cancer using PRISMA analysis. Journal of Drug Delivery Science and Technology, 66, 102865. https://doi.org/10.1016/j.jddst.2021.102865
- Wu, H.-C., Tsai, C.-C., Hsu, P.-C., Kuo, C.-Y. (2025). Herbal Medicine in Breast Cancer Therapy: Mechanisms, Evidence, and Future Perspectives. Current Issues in Molecular Biology, 47 (5), 362. https://doi.org/10.3390/cimb47050362
- Akhlaghi, M., Taebpour, M., Lotfabadi, N. N., Naghib, S. M., Jalili, N., Farahmand, L. et al. (2022). Synthesis and characterization of smart stimuli-responsive herbal drug-encapsulated nanoniosome particles for efficient treatment of breast cancer. Nanotechnology Reviews, 11 (1), 1364–1385. https://doi.org/10.1515/ntrev-2022-0080
- Gupta, R., Mishra, P. S., Kala, N., Pai, A., Malviya, R. (2021). Therapeutic Potential of Herbal Molecules against Breast Cancer. Current Nutrition & Food Science, 17 (7), 652–661. https://doi.org/10.2174/1573401317666210111110556
- Kumar, S., Gupta, A., Gauttam, V., Sharma, K., Deepak, A., Thakur, R. (2023). Important role of herbal extracts in the management of breast cancer. International Journal of Ayurveda and Pharma Research, 11 (10), 92–100. https://doi.org/10.47070/ijapr.v11i10.3003
- T. Karthiyayini, T. K., B. Diviniya, B. D., N. Jeyavarthani, N. J., S. Ragaswetha, S. R., M.Sneka, M. S., R.Vishnupriya, R. V. (2025). Herbal Medicine: As a Complementary therapy to Traditional Treatment for Breast Cancer-A Systemic review. International Journal of Pharmaceutical Research and Applications, 10 (2), 1789–1796. https://doi.org/10.35629/4494-100217891796
- Omarbayeva, N. A., Kaidarova, D. R., Omarov, D. Kh., Askandirova, A., Keskin, Kh., Abdrakhmanova, A. Zh. et al. (2024). Prevention of tumors in treating fibrocystic breast diseases using Vitex agnus-castus-based herbal remedy. Tumors of Female Reproductive System, 20 (4), 62–69. https://doi.org/10.17650/1994-4098-2024-20-4-62-69
- Seksaria, K., Patial, D., Aneja, A., Arora, P., Kumar, S. (2026). Recent Advances in the Chemistry of Herbal Drugs for the Management of Breast Cancer: An Update. The Natural Products Journal, 16 (3). https://doi.org/10.2174/0122103155327969241128110431
- Rajput, S., Malviya, R., Srivastava, S., Ahmad, I., Obaidur Rab, S., Uniyal, P. (2025). In vivo Evaluation of Apoptosis-Inducing Herbs for the Treatment of Breast Cancer: Recent Developments and Mechanism of Action. Current Nutrition & Food Science, 21 (3), 282–294. https://doi.org/10.2174/0115734013303288240730061019
- Shree, D., Patra, C. N., Sahoo, B. M. (2025). Current Insights into Polymeric Nanocarriers for Delivery of Phytomedicines in Breast Cancer Therapy. Current Nanomaterials, 10. https://doi.org/10.2174/0124054615358250250709130728
- Anago, A. D., Gaetan Segbo, J. A., Gnangnon, F., Akpovi, C. D., Agbangla, C. (2023). Some Medicinal Plants with Anti-breast Cancer Activity and the Input of Phytotherapy in the Treatment of Breast Cancer. European Scientific Journal, ESJ, 19 (18), 66. https://doi.org/10.19044/esj.2023.v19n18p66
- Zhang, S., Guo, L., Tao, R., Liu, S. (2024). Ferroptosis-targeting drugs in breast cancer. Journal of Drug Targeting, 33 (1), 42–59. https://doi.org/10.1080/1061186x.2024.2399181
- Mostary, S., Hossain Khan, M. M., Hossain, M. A. M., Maitra, T. K. (2021). Response to different medical treatment options for mastalgia in fibrocystic breast disease. BIRDEM Medical Journal, 12 (1), 22–29. https://doi.org/10.3329/birdem.v12i1.57221
- Shahcheraghi, S., Sardar, H., Lotfi, M., Khan, H. (2025). The effect of crocin on the proliferation, inflammation, drug synergism, and angiogenesis in breast cancer. Phytonutrients, 4 (1), 1–7. https://doi.org/10.62368/pn.v4i1.45
- Wu, Z.-Y., Qiu, K.-Y., Gai, Y.-J., Wu, J.-H., Zhou, B.-X., Shi, Q.-F. (2025). Quercetin: A Natural Ally in Combating Breast Cancer. International Journal of Nanomedicine, 20, 9155–9177. https://doi.org/10.2147/ijn.s518174
- San, S. H., Ngai, S. C. (2025). The synergistic anticancer effects of curcumin in combination with breast cancer chemotherapy drugs. Life Sciences, Medicine and Biomedicine, 9 (1). https://doi.org/10.28916/lsmb.9.1.2025.173
- O’Shaughnessy, J., Sousa, S., Cruz, J., Fallowfield, L., Auvinen, P., Pulido, C. et al. (2021). Preference for the fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection in patients with HER2-positive early breast cancer (PHranceSCa): A randomised, open-label phase II study. European Journal of Cancer, 152, 223–232. https://doi.org/10.1016/j.ejca.2021.03.047
- Xu, B., Yan, M., Ma, F., Hu, X., Feng, J., Ouyang, Q. et al. (2021). Pyrotinib plus capecitabine versus lapatinib plus capecitabine for the treatment of HER2-positive metastatic breast cancer (PHOEBE): a multicentre, open-label, randomised, controlled, phase 3 trial. The Lancet Oncology, 22 (3), 351–360. https://doi.org/10.1016/s1470-2045(20)30702-6
- Yu, K.-D., Ye, F.-G., He, M., Fan, L., Ma, D., Mo, M. et al. (2020). Effect of Adjuvant Paclitaxel and Carboplatin on Survival in Women With Triple-Negative Breast Cancer. JAMA Oncology, 6 (9), 1390–1396. https://doi.org/10.1001/jamaoncol.2020.2965
- Mir, M. (2025). Retinoids as anti-cancer agents in breast cancer: A new hope for breast cancer treatment. Elsevier. https://doi.org/10.1016/C2024-0-02560-X
- Colaco, V., Datta, D., Kudarha, R., Singh, A. K., Dhas, N. (2025). Microneedles as Gateways: Smart Nanoparticle Delivery for Enhanced Breast Cancer Treatment. ACS Omega, 10 (37), 42135–42150. https://doi.org/10.1021/acsomega.5c04565
- Jurj, E.-D., Colibășanu, D., Vasii, S.-O., Suciu, L., Dehelean, C. A., Udrescu, L. (2025). Redefining Breast Cancer Care by Harnessing Computational Drug Repositioning. Medicina, 61 (9), 1640. https://doi.org/10.3390/medicina61091640
- Rajnani, N., Kurup, N. (2025). Development of Methotrexate-Loaded Nanocochleates for Treatment of Breast Cancer by Trapping Method. Research Journal of Pharmacy and Technology, 18 (9), 4384–4388. https://doi.org/10.52711/0974-360x.2025.00628
- Li, J. (2025). Research of Nanoparticle Drug Delivery System of Breast Cancer. Highlights in Science, Engineering and Technology, 125, 321–328. https://doi.org/10.54097/03ddmk58
- Bolledla, N., Bakshi, V. (2025). Development of abemaciclib-encapsulated nanosponges for breast cancer: optimization, drug release kinetics, and in vitro efficacy. Journal of Applied Pharmaceutical Research, 13 (4), 279–297. https://doi.org/10.69857/joapr.v13i4.1234
- Ahmadi, S., Seraj, M., Chiani, M., Hosseini, S., Bazzazan, S., Akbarzadeh, I. et al. (2022). In vitro Development of Controlled-Release Nanoniosomes for Improved Delivery and Anticancer Activity of Letrozole for Breast Cancer Treatment. International Journal of Nanomedicine, 17, 6233–6255. https://doi.org/10.2147/ijn.s384085
- Kumari, M., Sharma, N., Manchanda, R., Gupta, N., Syed, A., Bahkali, A. H., Nimesh, S. (2021). PGMD/curcumin nanoparticles for the treatment of breast cancer. Scientific Reports, 11 (1). https://doi.org/10.1038/s41598-021-81701-x
- Juan, A., Cimas, F. J., Bravo, I., Pandiella, A., Ocaña, A., Alonso-Moreno, C. (2020). Antibody Conjugation of Nanoparticles as Therapeutics for Breast Cancer Treatment. International Journal of Molecular Sciences, 21 (17), 6018. https://doi.org/10.3390/ijms21176018
- Behl, A., Chhillar, A. K. (2023). Nano-Based Drug Delivery of Anticancer Chemotherapeutic Drugs Targeting Breast Cancer. Recent Patents on Anti-Cancer Drug Discovery, 18 (3), 325–342. https://doi.org/10.2174/157489281703220610170559
- Mi, X., Hu, M., Dong, M., Yang, Z., Zhan, X., Chang, X. et al. (2021). Folic Acid Decorated Zeolitic Imidazolate Framework (ZIF-8) Loaded with Baicalin as a Nano-Drug Delivery System for Breast Cancer Therapy. International Journal of Nanomedicine, 16, 8337–8352. https://doi.org/10.2147/ijn.s340764
- Chukhraev, N., Zukow, W., Vladimirova, N., Chukhraeva, E., Tereshchenko, O. (2022). Complementary methods for the prevention and treatment of stress-induced mastopathy. Journal of Education, Health and Sport, 12 (8), 107–122. https://doi.org/10.12775/jehs.2022.12.08.011
- Zavizion, V. F. (2024). Fibrocystic changes of the mammary glands: interpretation of the diagnosis, issues of diagnosis and treatment (Literature review). Reproductive health of woman, 2, 96–102. https://doi.org/10.30841/2708-8731.2.2024.304668
- Podolskyi, Vl. V., Podolskyi, V. V. (2021). Modern approaches to the treatment of mastopathy and correction of hyperestrogenic conditions in women of fertile age. Reproductive Health of Woman, 3, 65–70. https://doi.org/10.30841/2708-8731.3.2021.234247
- Zuikina, S., Vyshnevska, L., Sydora, N., Semchenko, K., Kovalova, T., Bohutska, O. (2021). To the issue of distribution and modern pharmacocorection of mastopathy in Ukraine and the world: review. Pharmacology OnLine, 3, 156–169. Available at: https://pharmacologyonline.silae.it/files/archives/2021/vol3/PhOL_2021_3_A019_Zuikina.pdf
- Sokolik, O. P., Prozorova, G. O. (2022). Current research opportunities for potential phytotherapeutic agents for the treatment of pathologies of the female reproductive system. European Journal of Clinical and Experimental Medicine, 20 (1), 109–116. https://doi.org/10.15584/ejcem.2022.1.15
- Bobritska, V. V., Strakhovetsky, V. S., Golovina, O. V., Kozub, T. O. (2024). Impact on the links of the mastopathy pathogenesis: a view on the pathological cascade correction. Reproductive Endocrinology, 71, 72–83. https://doi.org/10.18370/2309-4117.2024.71.72-83
- Yadav, P., Kumar, A., Sherkhane, R., Sharma, A. (2025). Fibrocystic breast disease in ayurveda: a review. International Journal of Research in Ayurveda and Pharmacy, 16 (2), 162–165. https://doi.org/10.7897/2277-4343.16264
- Alipour, S., Rastad, H., Saberi, A., Faiz, F., Maleki-Hajiagha, A., Abedi, M. (2021). Metformin in the management of fibrocystic breast disease: a placebo-controlled randomized clinical trial. DARU Journal of Pharmaceutical Sciences, 29 (2), 389–396. https://doi.org/10.1007/s40199-021-00424-6
- Yeszhan, B. G., Ossikbayeva, S. O. (2021). Study of danazol active agent effect on Mcf10a breast cells redox phosphorylation. Oncologia i Radiologia Kazakhstana, 60 (2), 32–35. https://doi.org/10.52532/2521-6414-2021-2-60-32-35
- Guseynov, A., D’yakov, M. (2024). Assessment of the effectiveness of young maston in the conservative treatment of fibrocystic mastopathy in women of reproductive age. Clinical Medicine and Pharmacology, 10 (1), 2–5. https://doi.org/10.12737/2409-3750-2024-10-1-2-5
- Saadat, M. A., Aslam, Md. M., Akanda, Md. S. (2022). A Comparative Study of Danazol alone with Danazol Combined with Evening Primrose Oil in the Treatment of Fibrocystic Breast Disease. SAS Journal of Surgery, 8 (11), 696–701. https://doi.org/10.36347/sasjs.2022.v08i11.007
- Godazandeh, G., Ala, S., Motlaq, T. M., Sahebnasagh, A., Bazi, A. (2021). The comparison of the effect of flaxseed oil and vitamin E on mastalgia and nodularity of breast fibrocystic: a randomized double-blind clinical trial. Journal of Pharmaceutical Health Care and Sciences, 7 (1). https://doi.org/10.1186/s40780-020-00186-4
- Meliboyeva S. S. Q., Boltayev M. M., Sharipova E. M., Sharipova R. G. (2021). Comparative efficiency of the preparation "Nodinorm" in complex treatment of fibrocystic mastopathy. An International Multidisciplinary Research Journal, 11 (10), 1591–1596.
- Dolatshahi, K., Mosaheb, S. A., Foodani, M. N., Hosseininezahdian, S., Esfahan, S. Z. (2024). Effects of Melatonin Supplementation on Clinical Symptoms and Paraclinical Outcomes in Women Diagnosed With Fibrocystic Breast Disease: An Interventional Study. Acta Medica Iranica, 61 (11), 691–698. https://doi.org/10.18502/acta.v61i11.16081
- Zuikina, S., Vyshnevska, L. (2020). Research of quality indicators and stability of herbal species for mastopathy therapy. Ukrainian Biopharmaceutical Journal, 1 (62), 30–36. https://doi.org/10.24959/ubphj.20.261
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Polina Palyvoda, Svitlana Zuikina, Volodymyr Yakovenko, Liubov Bodnar, Oleksandr Shmalko

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.






