Effects of non-steroidal anti-inflammatory agents on systemic hemostasis during the most acute period of cold injury in rats
DOI:
https://doi.org/10.15587/2519-4852.2023.294311Keywords:
acute general cooling, diclofenac sodium, etoricoxib, blood coagulation, experimentAbstract
Non-steroidal anti-inflammatory drugs (NSAIDs) have recently been considered promising agents for the prevention and treatment of cold injuries. The results of previous studies demonstrate a distinct frigoprotective effect of diclofenac sodium and etoricoxib.
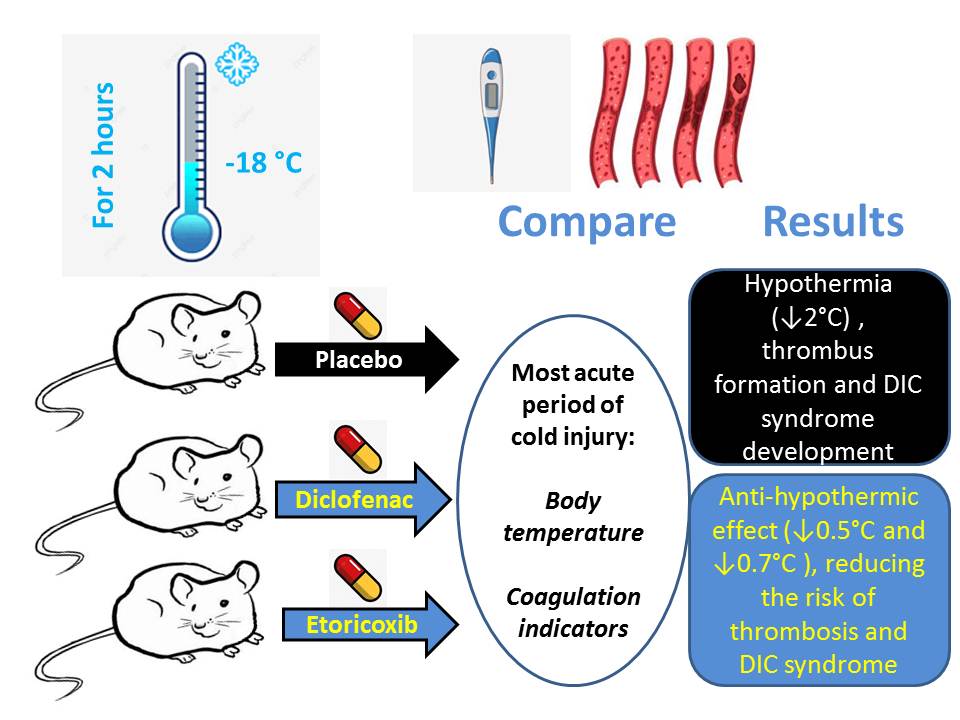
The aim of the study: to assess the impact of diclofenac sodium and etoricoxib, as the most effective frigoprotectors among NSAIDs, on coagulation indicators during the most acute phase of cold injuries using an acute model of general cooling in rats.
Materials and Methods: The experiment was carried out using 41 outbreed male rats weighing 310±10 g. Cold injury was induced by acute general cooling (exposure to –18 °C for 2 hours). Diclofenac sodium (7 mg/kg) and etoricoxib (5 mg/kg) were administered intragastrically 30 minutes before the onset of cold exposure. Rectal temperature was measured before and after cold exposure. Immediately after exposure, plasma was used to determine prothrombin time (PT), thrombin time (TT), activated partial thromboplastin time (APTT), fibrinogen levels, and in blood serum – the residual amount of prothrombin, thrombin, fibrinogen, as well as D-dimer using species-specific immunoenzymatic analysis kits.
Results: Etoricoxib and especially diclofenac sodium significantly reduced the degree of hypothermia (rectal temperature decreased by 1.3 % and 1.9 %, respectively, compared to a 5.4 % decrease in the control group, p < 0.05). In the acute phase of cold injury in the untreated control group, there was a significant increase in D-dimer (by 2.7 times) and fibrinogen content (by 1.9 times) in blood serum, alongside a 21.7 % increase in thrombin time, indicating a heightened risk of thrombus formation and DIC syndrome development. The other coagulation indicators did not show significant changes. Both diclofenac sodium and etoricoxib significantly reduced elevated D-dimer and serum fibrinogen, normalizing thrombin time and indicating an antithrombotic effect. There was no significant difference in the effect of both NSAIDs on blood coagulation status.
Conclusions: The acute phase of cold injury demonstrates a dangerous shift in blood coagulation towards thrombus formation and DIC syndrome development. Prophylactic use of diclofenac sodium and, to a lesser extent, etoricoxib displays an anti-hypothermic effect, reducing the risk of thrombosis and DIC syndrome. This proves the expediency of using these NSAIDs for acute cold injury
Supporting Agency
- “Experimental substantiation for improving the effectiveness of prevention and treatment of cold injuries” of the list of scientific studies of the Ministry of Health of Ukraine, carried out at the expense of the state budget of Ukraine No. 0120u102460 (Order of the Ministry of Health of Ukraine No. 2651 of 17.11.2020)
References
- QuickStats: Death Rates Attributed to Excessive Cold or Hypothermia Among Persons Aged ≥15 Years, by Urban-Rural Status and Age Group – National Vital Statistics System, United States, 2019 (2021). MMWR Morb Mortal Wkly Rep, 70 (7), 258. doi: http://doi.org/10.15585/mmwr.mm7007a6
- Yak unyknuty pereokholodzhennia: nahaduiemo osnovni pravyla povedinky u kholod (2019). MOZ Ukrainy. Available at: https://moz.gov.ua/article/news/jak-uniknuti-pereoholodzhennja-nagaduemo-osnovni-pravila-povedinki-u-holod
- Cold Weather Injuries, Active and Reserve Components, U.S. Armed Forces (2019). Available at: https://www.health.mil/News/Articles/2019/11/01/Cold-Weather-Injuries
- Fudge, J. (2016) Exercise in the Cold: Preventing and Managing Hypothermia and Frostbite Injury. Sports Health, 8 (2), 133–139. doi: http://doi.org/10.1177/1941738116630542
- Gross, E., Moore, J. (2012). Using thrombolytics in frostbite injury. Journal of Emergencies, Trauma, and Shock, 5 (3), 267––271. doi: http://doi.org/10.4103/0974-2700.99709
- Kapelka, І. G., Shtrigol, S. Iu. (2019). The comparative research of frigoprotective properties of nonsteroidal anti-inflammatory drugs оn the model of acute general cooling. Pharmacology and Drug Toxicolog, 13 (5), 338–343.
- Kapelka, I. H., Shtryhol, S. Yu., Lesyk, R. B., Lozynskyi, A. V., Khom’iak, S. V., Novikov, V. P. (2020). The comparative research of arachidonic acid cascade inhibitors for frigoprotective activity. Pharmacology and Drug Toxicology, 14 (2), 122–128. doi: http://doi.org/10.33250/14.02.122
- Kapelka, I. G., & Shtrygol’, S. Yu. (2020). The characteristics of the anti-inflammatory action of sodium diclofenac in cold and normal environment. News of Pharmacy, 2 (100), 106–112. doi: http://doi.org/10.24959/nphj.20.37
- Kapelka, I., Shtrygol, S., Koiro, O., Merzlikin, S., Kudina, O., Yudkevych, T. (2021). Effect of arachidonic acid cascade inhibitors on body temperature and cognitive functions in rats in the Morris water maze after acute cold injury. Pharmazie, 76 (7), 313–316.
- Shtrygol’, S., Koiro, O., Kudina, O., Tovchiga, O., Yudkevych, T., Oklei, D. (2022). The influence of non-steroidal anti-inflammatory drugs with different mechanisms of action on the course of stress reaction, the functional state of kidneys, liver, and heart on the model of acute general cooling. ScienceRise: Pharmaceutical Science, 2 (36), 46–55. doi: http://doi.org/10.15587/2519-4852.2022.255797
- Shtrygol’, S. Yu., Koiro, O. O., Kudina, O. V., Yudkevych, T. K., Gorbach, T. V. (2022). Comparative analysis of the effect of diclofenac sodium and etoricoxib on energy metabolism in rat liver in the acute general cooling model. Medicni Perspektivi, 27 (4), 51–57. doi: http://doi.org/10.26641/2307-0404.2022.4.271171
- Shtrygol, S., Tovchiga, O., Kudina, O., Koiro, O., Yudkevich, T., Gorbach, T. (2022). The effect of non-steroidal anti-inflammatory drugs with different mechanisms of action on the body temperature and cyclooxygenase pathway of the arachidonic acid cascade on the model of acute general cooling (air hypothermia) in rats. Česká a Slovenská Farmacie, 71 (5), 214–223. doi: http://doi.org/10.5817/csf2022-5-214
- Yukhymchuk, A. V., Voloshchuk, N. I., Shtrygol, S. Yu. (2023). Vplyv hliukozaminu na stan systemy zghortannia krovi u samtsiv ta samok shchuriv za hostroi kholodovoi travmy. Klinichna farmakolohiia sohodennia: shliakhy maksymalnoi dopomohy likarskii spetsialnosti. Vinnytsia, 170–172.
- Jin, H.-X., Teng, Y., Dai, J., Zhao, X.-D. (2021). Expert consensus on the prevention, diagnosis and treatment of cold injury in China, 2020. Military Medical Research, 8 (1). doi: http://doi.org/10.1186/s40779-020-00295-z
- Bondarev, Ye. V., Shtrygol, S. Yu., Zupanets, I. A., Otrishko, I. A. (2017). Platelet aggregation under the action of drugs of glucosamine hydrochloride and acetylsalicylic acid in acute cold injury. Clinical pharmacy, 21 (1), 50–56. doi: http://doi.org/10.24959/cphj.17.1411
- Sachs, C., Lehnhardt, M., Daigeler, A., Goertz, O. (2015). The Triaging and Treatment of Cold-Induced Injuries. Deutsches Ärzteblatt International, 112 (44), 741–747. doi: http://doi.org/10.3238/arztebl.2015.0741
- Bondariev, Ye. V., Shtrygol, S. Yu., Drohovoz, S. M., Shchokina, K. H. (2018). Kholodova travma: doklinichne vyvchennia likarskykh preparativ z fryhoprotektornymy vlastyvostiamy. Kharkiv: Natsionalnyi farmatsevychnyi universytet, 35.
- Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the protection of animals used for scientific purposes (2010). Available at: https://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX%3A32010L0063
- Weiner, M. (1958). Residual Serum Thrombin Activity. Clinical Chemistry, 4 (4), 271–277. doi: http://doi.org/10.1093/clinchem/4.4.271
- Shapovalov, K. G. (2008). Endotelialnaya sekretsiya vazoaktivnyih molekul pri holodovoy travme konechnostey. Travmatol. Ortopediya, 2 (48), 53–56.
- Adelborg, K., Larsen, J. B., Hvas, A. (2021). Disseminated intravascular coagulation: epidemiology, biomarkers, and management. British Journal of Haematology, 192 (5), 803–818. doi: http://doi.org/10.1111/bjh.17172
- Bondariev, Ye. V. (2020). Eksperymentalne obgruntuvannia optymizatsii profilaktyky ta likuvannia kholodovoi travmy zasobamy metabolitotropnoi ta protyzapalnoi dii. Kharkiv: Natsionalnyi farmatsevtychnyi universytet, 431.
- Rathjen, N. A., Shahbodaghi, S. D., Brown, J. A. (2019). Hypothermia and Cold Weather Injuries. American Family Physician, 100 (11), 680–686.
- Mohr, J. P., Choi, D. W., Wolf, Ph. A. et al. (2004). Stroke. Pathophysiology, diagnosis, and management. Churchill Livingstone. Available at: doi: http://doi.org/10.1016/B0-443-06600-0/X5001-9
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Sergiy Shtrygol’, Andrii Taran, Tetiana Yudkevych, Dmytro Lytkin, Iryna Lebedinets, Polina Chuykova, Olga Koiro

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.






