Acute heat trauma model in rats, gender-dependent thermoresistance, and screening of potential thermoprotectors
DOI:
https://doi.org/10.15587/2519-4852.2024.301620Keywords:
acute heat trauma, hyperthermia, thermoresistance, gender, glucosamine hydrochloride, non-steroidal anti-inflammatory drugs, experimentAbstract
Heat trauma (HT) is an urgent medical and social problem. Heat damage is a widespread effect of the environment on humans, driven by global warming, military conflicts, technological disasters, work in hot environments, and engagement in extreme sports and tourism.
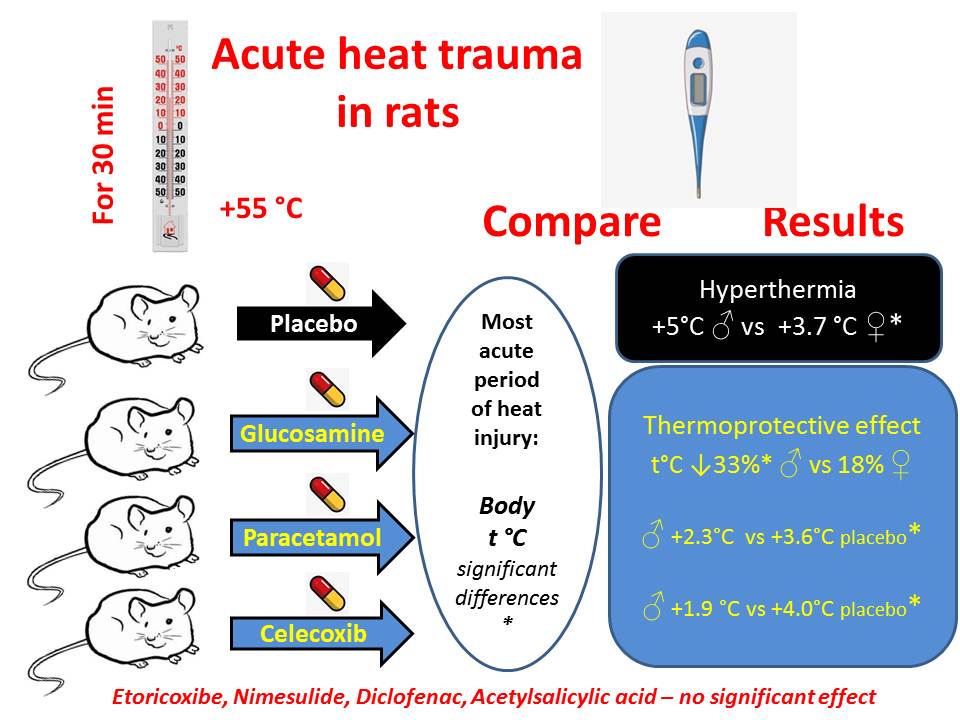
The aim of the study: to propose a model of acute HT in rats that does not cause the death of animals, to determine the dependence of thermoresistance on gender, and to compare the effectiveness of the thermoprotective effects of a range of non-steroidal anti-inflammatory drugs (NSAIDs), paracetamol, and glucosamine hydrochloride in this model.
Materials and Methods: The experiment was conducted on adult white rats of both genders. Acute HT was modelled by using a specially developed method involving heat exposure to animals at +55 °C for 30 minutes, followed by a recovery period of 60 minutes. Rectal temperature was measured every 15 minutes. The degree of hyperthermia in males and females was determined. The presence and intensity of the thermoprotective effect of glucosamine hydrochloride (G h/ch), diclofenac sodium, acetylsalicylic acid (ASA), nimesulide, etoricoxib, celecoxib, and paracetamol were evaluated through intragastric administration 60 minutes before heat exposure. The results were analyzed using the STATISTICA 12.0 program.
Results: It was established that heat exposure at +55 °C for 30 minutes effectively replicates acute HT in rats without causing animal fatalities, adhering to bioethical requirements. Body temperature increases by 10-13 %, characterized as a heat stroke. Occasionally, thermoresistant animals are encountered, where the temperature increase during the first 15 minutes of exposure is less than 1 °C. These animals should not be used for further modelling of heat trauma. Male rats are more sensitive to the effect of high environmental temperatures than females, exhibiting greater hyperthermia (temperature increase of 5.03±0.39°C compared to 3.72±0.22 °C in females, p<0.01). The thermoprotective effect of glucosamine hydrochloride depends on gender, being more pronounced in males. Among the 6 tested COX inhibitors, the most significant thermoprotective effect was observed in the highly selective COX-2 inhibitor celecoxib and the weakly selective central inhibitor paracetamol, warranting in-depth research into their impact on organ and system states following heat trauma, as well as the mechanisms of their thermoprotective action. The thermoprotective effect is not associated with selectivity towards COX (cyclooxygenase): it is not observed in the highly selective COX-2 inhibitor etoricoxib and moderately selective COX-2 inhibitor nimesulide, as well as in non-selective COX inhibitors such as diclofenac sodium and aspirin, which also slows down the recovery of body temperature after heat exposure.
Conclusions: A convenient and simple model of acute HT in rats is proposed, demonstrating higher thermosensitivity and a more pronounced thermoprotective effect of glucosamine hydrochloride in males. A significant thermoprotective effect was identified in celecoxib and paracetamol, surpassing other investigated NSAIDs. The mechanism and specific features of this effect require further clarification
References
- Atlas of Mortality and Economic Losses from Weather, Climate and Water Extremes (1970–2019) (2021). World Meteorological Organization, No. 1267.
- Lu, R., Xu, K., Chen, R., Chen, W., Li, F., Lv, C. (2023). Heat waves in summer 2022 and increasing concern regarding heat waves in general. Atmospheric and Oceanic Science Letters, 16 (1), 100290. https://doi.org/10.1016/j.aosl.2022.100290
- Ballester, J., Quijal-Zamorano, M., Méndez Turrubiates, R. F., Pegenaute, F., Herrmann, F. R., Robine, J. M. et al. (2023). Heat-related mortality in Europe during the summer of 2022. Nature Medicine, 29 (7), 1857–1866. https://doi.org/10.1038/s41591-023-02419-z
- Nybo, L., Rasmussen, P., Sawka, M. N. (2014). Performance in the Heat—Physiological Factors of Importance for Hyperthermia‐Induced Fatigue. Comprehensive Physiology, 657–689. https://doi.org/10.1002/cphy.c130012
- Bondar, M. V., Pylypenko, M. M., Ovsiienko, T. V., Nevmerzhytskyi I. M. (2018). Hipertermichni syndromy: etiolohiia, patohenez, diahnostyka ta intensyvna terapiia. Medytsyna nevidkladnykh staniv, 2 (89).
- Pryor, R. R., Casa, D. J., Holschen, J. C., O’Connor, F. G., Vandermark, L. W. (2013). Exertional Heat Stroke: Strategies for Prevention and Treatment From the Sports Field to the Emergency Department. Clinical Pediatric Emergency Medicine, 14 (4), 267–278. https://doi.org/10.1016/j.cpem.2013.10.005
- Pro zatverdzhennia ta vprovadzhennia medyko-tekhnolohichnykh dokumentiv zi standartyzatsii ekstrenoi medychnoi dopomohy (2019). Nakaz MOZ Ukrainy No. 1269. 05.06.2019. Available at: https://zakon.rada.gov.ua/go/v1269282-19 Last accessed: 22.02.2024
- Faiumi, Kh. A. D., Shtryhol, S. Yu., Zupanets, I. A., Tovchyha, O. V., Koiro, O. O. (2016). Pat. No. 110629. Zastosuvannia hliukozaminu hidrokhlorydu yak zasobu, shcho zakhyshchaie orhanizm vid systemnoho vplyvu vysokykh temperatur. MPK: (2016.01) A61K 31/726 (2006.01), A61P 43/00. No. a201308217; declareted: 01.07.2013; published: 25.01.2016, Bul. No. 2, 6.
- Koiro, O. O., Shtryhol, S. Yu. (2017). Hliukozaminu hidrokhloryd yak perspektyvnyi termoprotektor. V Natsionalnyi zizd farmakolohiv Ukrainy. Zaporizhzhia, 64.
- Fedorov, V. N. (1999). Farmakodinamika adaptogenov: eksperimentalnoe i klinicheskoe issledovanie. [PhD theses; Moscow].
- Sharma, H. S. (2007). Methods to produce hyperthermia-induced brain dysfunction. Neurobiology of Hyperthermia, 162, 173–199. https://doi.org/10.1016/s0079-6123(06)62010-4
- Damanhouri, Z. A., Tayeb, O. S. (1992). Animal models for heat stroke studies. Journal of Pharmacological and Toxicological Methods, 28 (3), 119–127. https://doi.org/10.1016/1056-8719(92)90073-a
- Bondariev, Ye. V. (2011). Stattevi vidminnosti chutlyvosti myshei do hostroho okholodzhennia. Farmakom, 1/2, 79–81.
- Voloshchuk, N. I., Yuhimchuk, A. V. (2023). Sex peculiarities of survival of animals with acute cold injury and correction with glucosamine hydrochloride. Pharmacology and Drug Toxicology, 17 (4), 248–254.
- Yevropeiska konventsiia pro zakhyst khrebetnykh tvaryn, shcho vykorystovuiutsia dlia doslidnykh ta inshykh naukovykh tsilei (1986). Konventsiia; Rada Yevropy 18.03.1986. Available at: https://zakon.rada.gov.ua/go/994_137 Last accessed: 22.02.2024
- Pro zakhyst tvaryn vid zhorstokoho povodzhennia (2006). Zakon Ukrainy No. 3447-IV. 21.02.2006. Available at: https://zakon.rada.gov.ua/go/3447-15 Last accessed: 22.02.2024
- Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the protection of animals used for scientific purposes (2010). Available at: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2010:276:0033:0079:en:PDF
- Botting, R. M. (2000). Mechanism of Action of Acetaminophen: Is There a Cyclooxygenase 3? Clinical Infectious Diseases, 31 (5), S202–S210. https://doi.org/10.1086/317520
- Graham, G. G., Scott, K. F. (2005). Mechanism of Action of Paracetamol. American Journal of Therapeutics, 12 (1), 46–55. https://doi.org/10.1097/00045391-200501000-00008
- Graham, G. G., Davies, M. J., Day, R. O., Mohamudally, A., Scott, K. F. (2013). The modern pharmacology of paracetamol: therapeutic actions, mechanism of action, metabolism, toxicity and recent pharmacological findings. Inflammopharmacology, 21 (3), 201–232. https://doi.org/10.1007/s10787-013-0172-x
- Kapelka, I. G., Shtrygol’, S. Yu. (2019). The comparative research of frigoprotective properties of nonsteroidal anti-inflammatory drugs оn the model of acute general cooling. Pharmacology and Drug Toxicologу, 13 (5), 338–343. https://doi.org/10.33250/13.05.338
- Kapelka, I. H., Shtryhol, S. Yu., Lesyk, R. B., Lozynskyi, A. V., Khomiak, S. V., Novikov, V. P. (2020). The comparative research of arachidonic acid cascade inhibitors for frigoprotective activity. Pharmacology and Drug Toxicologу, 14 (2), 122–128. https://doi.org/10.33250/14.02.122
- Refinetti, R., Ma, H., Satinoff, E. (1990). Body temperature rhythms, cold tolerance, and fever in young and old rats of both genders. Experimental Gerontology, 25 (6), 533–543. https://doi.org/10.1016/0531-5565(90)90019-x
- Yuhimchuk, A. V., Voloshchuk, N. I., Shtrygol, S. Yu., Nefodov, O. O., Piliponova, V. V., Oliinyk, Yu. M. et al. (2023). Vascular mechanisms in the formation of gender differences in the protective effect of glucosamine in experimental cold injury. World of Medicine and Biology, 19 (86), 243–247. https://doi.org/10.26724/2079-8334-2023-4-86-243-247
- Davis, W. M., Pharm, B. S. (1998). Impact of gender on drug responses. Drug topics, 91–101.
- Kapelka, I., Shtrygol, S., Koiro, O., Merzlikin, S., Kudina, O., Yudkevych, T. (2021). Effect of arachidonic acid cascade inhibitors on body temperature and cognitive functions in rats in the Morris water maze after acute cold injury. Pharmazie, 76 (7), 313–316.
- Shtrygol’, S., Koiro, O., Kudina, O., Tovchiga, O., Yudkevych, T., Oklei, D. (2022). The influence of non-steroidal anti-inflammatory drugs with different mechanisms of action on the course of stress reaction, the functional state of kidneys, liver, and heart on the model of acute general cooling. ScienceRise: Pharmaceutical Science, 2 (36), 46–55. https://doi.org/10.15587/2519-4852.2022.255797
- Shtrygol’, S. Yu., Koiro, O. O., Kudina, O. V., Yudkevych, T. K., Gorbach, T. V. (2022). Comparative analysis of the effect of diclofenac sodium and etoricoxib on energy metabolism in rat liver in the acute general cooling model. Medicni Perspektivi, 27 (4), 51–57. https://doi.org/10.26641/2307-0404.2022.4.271171
- Shtrygol, S., Tovchiga, O., Kudina, O., Koiro, O., Yudkevich, T., Gorbach, T. (2022). The effect of non-steroidal anti-inflammatory drugs with different mechanisms of action on the body temperature and cyclooxygenase pathway of the arachidonic acid cascade on the model of acute general cooling (air hypothermia) in rats. Česká a Slovenská Farmacie, 71(5), 214–223. https://doi.org/10.5817/csf2022-5-214
- Anderson, B. J. (2008). Paracetamol (Acetaminophen): mechanisms of action. Pediatric Anesthesia, 18 (10), 915–921. https://doi.org/10.1111/j.1460-9592.2008.02764.x
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Polina Chuykova, Sergii Shtrygol’, Andrii Taran, Tetiana Yudkevych, Iryna Lebedinets, Denys Oklei

This work is licensed under a Creative Commons Attribution 4.0 International License.
Our journal abides by the Creative Commons CC BY copyright rights and permissions for open access journals.






