Лікопов’язані проблеми у коморбідних пацієнтів з тривожно-депресивними розладами
DOI:
https://doi.org/10.15587/2519-4852.2025.338127Ключові слова:
лікопов’язані проблеми, коморбідність, антидепресанти, заспокійливі препарати, поліпрагмазіяАнотація
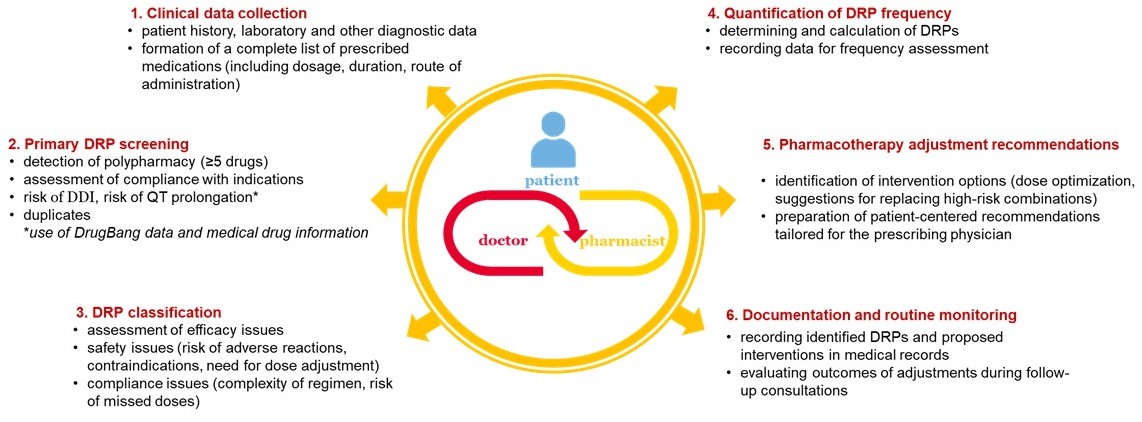
Лікопов’язані проблеми (ЛПП) становлять суттєву загрозу безпеці пацієнтів, особливо в умовах коморбідності та поліпрагмазії. ЛПП можуть виявлятись небажаними реакціями, взаємодією лікарських засобів тощо, потенційно негативно впливаючи на ефективність та безпеку лікування. Оскільки більшість ЛПП є потенційно передбачуваними за умови своєчасного виявлення та корекції фармакотерапії, зростає роль клінічного фармацевта, який може бути включений в міждисциплінарну команду спеціалістів і в рамках фармацевтичного консультування сприяти їх мінімізації.
Мета: Метою нашого дослідження було оцінити частоту та характер ЛПП у коморбідних пацієнтів з тривожно-депресивними розладами для формування моделі фармацевтичного консультування.
Матеріали та методи: Був проведений ретроспективний аналіз 55 історій хвороб коморбідних пацієнтів, які знаходились на стаціонарному лікуванні у терапевтичному відділенні багатопрофільної лікарні м. Києва і отримували лікування основного захворювання та тривожно-депресивних розладів. Більшість пацієнтів (67%) мали крім основного 3–4 супутні захворювання, в тому числі тривожно-депресивний розлад.
Аналіз потенційних міжмедикаментозних взаємодій проводився з використанням бази даних DrugBank та офіційних інструкцій для медичного застосування лікарських засобів.
Статистичний аналіз включав кореляційний аналіз для оцінки взаємозв’язків між змінними та порівняння якісних показників за допомогою χ²-критерію Пірсона. Рівень статистичної значущості приймався за p < 0,05. Обробку даних здійснювали із використанням пакету Microsoft Excel.
Результати: Загальна частота ЛПП на 1 пацієнта склала 3.73 ± 2.58, поліпрагмазії виявлено у 84% пацієнтів.
Виявлено достовірний кореляційний зв’язок (p < 0,05) між віком пацієнта і кількістю коморбідних станів (r = 0,48), а також між віком пацієнта і кількістю лікарських засобів, які він отримував (r = 0,45),
Достовірно частіше пацієнти отримували бензодіазепіни, ніж антидепресанти (89,1% проти 38,2%; χ² Пірсона = 30.80, p < 0,001).
Висновки: Серед коморбідних пацієнтів із тривожно-депресивними розладами, які перебували на лікуванні у соматичному стаціонарі, виявлено значну поширеність лікопов’язані проблем. Кількість лікарських засобів на курс лікування корелювала з віком пацієнтів. Практично всі пацієнти отримували бензодіазепіни, в тому числі більшість пацієнтів похилого віку, що є небезпечним через небезпеку наростання когнітивних порушень. Крім того, у 42% пацієнтів виявлено клінічно значущі міжмедикаментозні взаємодії, а у 29% – призначення препаратів при наявності обмежень або протипоказань. Результати дослідження акцентують важливість індивідуалізації фармакотерапії з урахуванням віку, коморбідності й потенційних взаємодій та обґрунтовують необхідність залучення клінічного фармацевта до мультидисциплінарної команди для мінімізації ризику виникнення лікопов’язаних проблем
Посилання
- Lekpittaya, N., Kocharoen, S., Angkanavisul, J., Siriudompas, T., Montakantikul, P., Paiboonvong, T. (2023). Drug-related problems identified by clinical pharmacists in an academic medical centre in Thailand. Journal of Pharmaceutical Policy and Practice, 17 (1). https://doi.org/10.1080/20523211.2023.2288603
- Kohn, L. T., Corrigan, J. M., Donaldson, M. S. (Eds.) (1999). To Err is Human: Building a Safer Health System. Washington: National Academy Press. https://doi.org/10.17226/9728
- Haag, J. D., Bellamkonda, V. R., Perinpam, L., Peters, B. J., Sunga, K. L., Gross, C. L. et al. (2022). Prevalence and Categorization of Drug-Related Problems in the Emergency Department. The Journal of Emergency Medicine, 63 (2), 192–199. https://doi.org/10.1016/j.jemermed.2022.04.016
- Garin, N., Sole, N., Lucas, B., Matas, L., Moras, D., Rodrigo-Troyano, A. et al. (2021). Drug related problems in clinical practice: a cross-sectional study on their prevalence, risk factors and associated pharmaceutical interventions. Scientific Reports, 11 (1). https://doi.org/10.1038/s41598-020-80560-2
- Pinho, L. G. de, Lopes, M. J., Correia, T., Sampaio, F., Arco, H. R. do, Mendes, A. et al. (2021). Patient-Centered Care for Patients with Depression or Anxiety Disorder: An Integrative Review. Journal of Personalized Medicine, 11(8), 776. https://doi.org/10.3390/jpm11080776
- Buist, E., McLelland, R., Rushworth, G. F., Stewart, D., Gibson-Smith, K., MacLure, A. et al. (2019). An evaluation of mental health clinical pharmacist independent prescribers within general practice in remote and rural Scotland. International Journal of Clinical Pharmacy, 41 (5), 1138–1142. https://doi.org/10.1007/s11096-019-00897-1
- Stuhec, M., Tement, V. (2021). Positive evidence for clinical pharmacist interventions during interdisciplinary rounding at a psychiatric hospital. Scientific Reports, 11 (1). https://doi.org/10.1038/s41598-021-92909-2
- Vitija, A., Amirthalingam, A., Soltani, A. (2022). The impact of digital interventions on medication adherence in paediatric populations with attention deficit hyperactivity disorder, depression, and/or anxiety: A rapid systematic review and meta-analysis. Research in Social and Administrative Pharmacy, 18 (12), 4017–4027. https://doi.org/10.1016/j.sapharm.2022.07.042
- Al Shakhori, M., Arain, S., Abdulsalim, S., Salim Karattuthodi, M., Al Dhamen, M., Almutairi, S. et al. (2025). Effectiveness of a pharmacist-led tele-psychiatric clinic in managing drug-related problems. Journal of Pharmaceutical Policy and Practice, 18 (1). https://doi.org/10.1080/20523211.2025.2460038
- Chudzicka-Czupała, A., Hapon, N., Chiang, S.-K., Żywiołek-Szeja, M., Karamushka, L., Lee, C. T. et al. (2023). Depression, anxiety and post-traumatic stress during the 2022 Russo-Ukrainian war, a comparison between populations in Poland, Ukraine, and Taiwan. Scientific Reports, 13 (1). https://doi.org/10.1038/s41598-023-28729-3
- Nehoda, T. S., Polova, Zh. M. (2024). methodological approaches to the formation of an optimal range of antidepressants for the inpatient treatment of martial law mental disorders. Health & Education, 1, 113–120. https://doi.org/10.32782/health-2024.1.15
- Antidepressants Global Market Report 2025 (2025). The Business Research Company. Available at: https://www.thebusinessresearchcompany.com/report/antidepressant-global-market-report
- PharmXplorer: Analytical system for pharmaceutical market monitoring in Ukraine. (2025). Available at: https://pharmxplorer.com.ua
- Kishi, T., Ikuta, T., Sakuma, K., Okuya, M., Hatano, M., Matsuda, Y., Iwata, N. (2022). Antidepressants for the treatment of adults with major depressive disorder in the maintenance phase: a systematic review and network meta-analysis. Molecular Psychiatry, 28 (1), 402–409. https://doi.org/10.1038/s41380-022-01824-z
- Solmi, M., Fornaro, M., Ostinelli, E. G., Zangani, C., Croatto, G., Monaco, F. et al. (2020). Safety of 80 antidepressants, antipsychotics, anti‐attention‐deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta‐review of 78 adverse effects. World Psychiatry, 19 (2), 214–232. https://doi.org/10.1002/wps.20765
- Woroń, J., Chrobak, A. A., Ślęzak, D., Siwek, M. (2022). Unprescribed and unnoticed: Retrospective chart review of adverse events of interactions between antidepressants and over-the-counter drugs. Frontiers in Pharmacology, 13. https://doi.org/10.3389/fphar.2022.965432
- Dobrea, C. M., Morgovan, C., Frum, A., Butuca, A., Chis, A. A., Arseniu, A. M. et al. (2025). The Assessment of the Safety Profile of Selective Serotonin Reuptake Inhibitors Versus Other Antidepressants: Drug–Drug Interaction Insights from EudraVigilance. Journal of Clinical Medicine, 14 (4), 1208. https://doi.org/10.3390/jcm14041208
- Demler, T. J. (2012). Psychiatric drug-drug interactions. US Pharmacist, 37 (11), 16–19. Available at: https://www.uspharmacist.com/article/psychiatric-drug-drug-interactions-a-refresher
- Hoffelt, C., Gross, T. (2016). A review of significant pharmacokinetic drug interactions with antidepressants and their management. Mental Health Clinician, 6 (1), 35–41. https://doi.org/10.9740/mhc.2016.01.035
- Milosavljevic, F., Bukvic, N., Pavlovic, Z., Miljevic, C., Pešic, V., Molden, E. et al. (2021). Association of CYP2C19 and CYP2D6 Poor and Intermediate Metabolizer Status With Antidepressant and Antipsychotic Exposure. JAMA Psychiatry, 78 (3), 270–280. https://doi.org/10.1001/jamapsychiatry.2020.3643
- Kee, P. S., Maggo, S. D. S., Kennedy, M. A., Chin, P. K. L. (2023). The pharmacogenetics of CYP2D6 and CYP2C19 in a case series of antidepressant responses. Frontiers in Pharmacology, 14. https://doi.org/10.3389/fphar.2023.1080117
- Classification for drug-related problems V8.01. (2018). Benelux: Europe PCN. Pharmaceutical Care Network Europe. Available at: https://www.pcne.org/upload/files/215_PCNE_classification_V8-01.pdf
- Viktil, K. K., Blix, H. S., Moger, T. A., Reikvam, A. (2006). Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug‐related problems. British Journal of Clinical Pharmacology, 63 (2), 187–195. https://doi.org/10.1111/j.1365-2125.2006.02744.x
- Hochhold, D., Nørgaard, L. S., Stewart, D., Weidmann, A. E. (2025). Identification, classification, and documentation of drug related problems in community pharmacy practice in Europe: a scoping review. International Journal of Clinical Pharmacy, 47(2), 247–269. https://doi.org/10.1007/s11096-024-01834-7
- Huiskes, V. J. B., van den Ende, C. H. M., Kruijtbosch, M., Ensing, H. T., Meijs, M., Meijs, V. M. M. et al. (2019). Effectiveness of medication review on the number of drug‐related problems in patients visiting the outpatient cardiology clinic: A randomized controlled trial. British Journal of Clinical Pharmacology, 86 (1), 50–61. Portico. https://doi.org/10.1111/bcp.14125
- Chance, E. A., Florence, D., Sardi Abdoul, I. (2024). The effectiveness of checklists and error reporting systems in enhancing patient safety and reducing medical errors in hospital settings: A narrative review. International Journal of Nursing Sciences, 11 (3), 387–398. https://doi.org/10.1016/j.ijnss.2024.06.003
- DiMatteo, M. R., Lepper, H. S., Croghan, T. W. (2000). Depression Is a Risk Factor for Noncompliance With Medical Treatment. Archives of Internal Medicine, 160 (14), 2101–2107. https://doi.org/10.1001/archinte.160.14.2101
- Wiersema, C., Oude Voshaar, R. C., van den Brink, R. H. S., Wouters, H., Verhaak, P., Comijs, H. C., Jeuring, H. W. (2022). Determinants and consequences of polypharmacy in patients with a depressive disorder in later life. Acta Psychiatrica Scandinavica, 146 (1), 85–97. https://doi.org/10.1111/acps.13435
- Alwhaibi, M. (2023). Inappropriate Medications Use and Polypharmacy among Older Adults with Anxiety Disorder. Journal of Clinical Medicine, 12 (13), 4195. https://doi.org/10.3390/jcm12134195
- Govaerts, J., Boeyckens, J., Lammens, A., Gilis, A., Bouckaert, F., De Hert, M. et al. (2021). Defining polypharmacy: in search of a more comprehensive determination method applied in a tertiary psychiatric hospital. Therapeutic Advances in Psychopharmacology, 11. https://doi.org/10.1177/20451253211000610
- DrugBank. Available at: https://go.drugbank.com
- Conn, D. K., Hogan, D. B., Amdam, L., Cassidy, K.-L., Cordell, P., Frank, C., Gardner, D. et al. (2020). Canadian Guidelines on Benzodiazepine Receptor Agonist Use Disorder Among Older Adults. Canadian Geriatrics Journal, 23 (1), 116–122. https://doi.org/10.5770/cgj.23.419
- Bonanno, E. G., Figueiredo, T., Mimoso, I. F., Morgado, M. I., Carrilho, J., Midão, L., Costa, E. (2025). Polypharmacy Prevalence Among Older Adults Based on the Survey of Health, Ageing and Retirement in Europe: An Update. Journal of Clinical Medicine, 14 (4), 1330. https://doi.org/10.3390/jcm14041330
- Kim, S., Lee, H., Park, J., Kang, J., Rahmati, M., Rhee, S. Y., Yon, D. K. (2024). Global and regional prevalence of polypharmacy and related factors, 1997–2022: An umbrella review. Archives of Gerontology and Geriatrics, 124, 105465. https://doi.org/10.1016/j.archger.2024.105465
- Simões, P. A., Santiago, L. M., Simões, J. A. (2020). Prevalence of polypharmacy in the older adult population within primary care in Portugal: a nationwide cross-sectional study. Archives of Medical Science, 20 (4), 1118–1127. https://doi.org/10.5114/aoms.2020.93537
- Bennie, M., Santa‐Ana‐Tellez, Y., Galistiani, G. F., Trehony, J., Despres, J., Jouaville, L. S. (2024). The prevalence of polypharmacy in older Europeans: A multi‐national database study of general practitioner prescribing. British Journal of Clinical Pharmacology, 90 (9), 2124–2136. https://doi.org/10.1111/bcp.16113
- Troncoso-Mariño, A., Roso-Llorach, A., López-Jiménez, T., Villen, N., Amado-Guirado, E., Fernández-Bertolin, S. et al. (2021). Medication-Related Problems in Older People with Multimorbidity in Catalonia: A Real-World Data Study with 5 Years’ Follow-Up. Journal of Clinical Medicine, 10 (4), 709. https://doi.org/10.3390/jcm10040709
- Lea, M., Mowe, M., Mathiesen, L., Kvernrød, K., Skovlund, E., Molden, E. (2019). Prevalence and risk factors of drug-related hospitalizations in multimorbid patients admitted to an internal medicine ward. PLOS ONE, 14 (7), e0220071. https://doi.org/10.1371/journal.pone.0220071
- Zhao, M., Chen, Z., Xu, T., Fan, P., Tian, F. (2023). Global prevalence of polypharmacy and potentially inappropriate medication in older patients with dementia: a systematic review and meta-analysis. Frontiers in Pharmacology, 14. https://doi.org/10.3389/fphar.2023.1221069
- Moßhammer, D., Haumann, H., Mörike, K., Joos, S. (2016). Polypharmacy – an Upward Trend with Unpredictable Effects. Deutsches Ärzteblatt International, 113, 627–233. https://doi.org/10.3238/arztebl.2016.0627
- Tor-Anyiin, A., Gwa, A., Okonkwo, R., Tor-Anyiin, I., Abuh, A. (2020). Prevalence and Perception of Pharmacists on Dispensing Prescription Only Medication without Prescription in Makurdi, Benue State, Nigeria. European Journal of Medical and Health Sciences, 2 (3). https://doi.org/10.24018/ejmed.2020.2.3.323
- Tan, H., Yan, X., Chen, Y., Huang, G., Luo, L., Li, W. et al. (2024). A real-world pharmacovigilance study of drug-induced QT interval prolongation: analysis of spontaneous reports submitted to FAERS. Frontiers in Cardiovascular Medicine, 11. https://doi.org/10.3389/fcvm.2024.1363382
- Gutlapalli, S. D., Prakash, K., Swarnakari, K. M., Bai, M., Manoharan, M. P., Raja, R. et al. (2022). The Risk of Fatal Arrhythmias Associated With Sertraline in Patients With Post-myocardial Infarction Depression. Cureus, 14 (9). https://doi.org/10.7759/cureus.28946
- Wang, C.-L., Wu, V., Huang, Y.-T., Chang, S. (2024). Abstract 4139536: Incidence of Severe QT Prolongation and the Assoicated Risk of Ventricular Arrhythmias and Sudden Cardiac Death in Patients Taking Antipsychotics or Antidepressants. Circulation, 150. https://doi.org/10.1161/circ.150.suppl_1.4139536
- van Westrhenen, R., Aitchison, K. J., Ingelman-Sundberg, M., Jukić, M. M. (2020). Pharmacogenomics of Antidepressant and Antipsychotic Treatment: How Far Have We Got and Where Are We Going? Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00094
##submission.downloads##
Опубліковано
Як цитувати
Номер
Розділ
Ліцензія
Авторське право (c) 2025 Kateryna Hoshtynar, Mykola Khaitovych, Oleksandr Kryvanych, Viktoriia Potaskalova

Ця робота ліцензується відповідно до Creative Commons Attribution 4.0 International License.
Наше видання використовує положення про авторські права Creative Commons CC BY для журналів відкритого доступу.