Devising a method for predicting a blood pressure level based on electrocardiogram and photoplethysmogram signals
DOI:
https://doi.org/10.15587/1729-4061.2022.265066Keywords:
blood pressure, machine learning, photoplethysmogram, bioelectric signals, pulse wave propagation timeAbstract
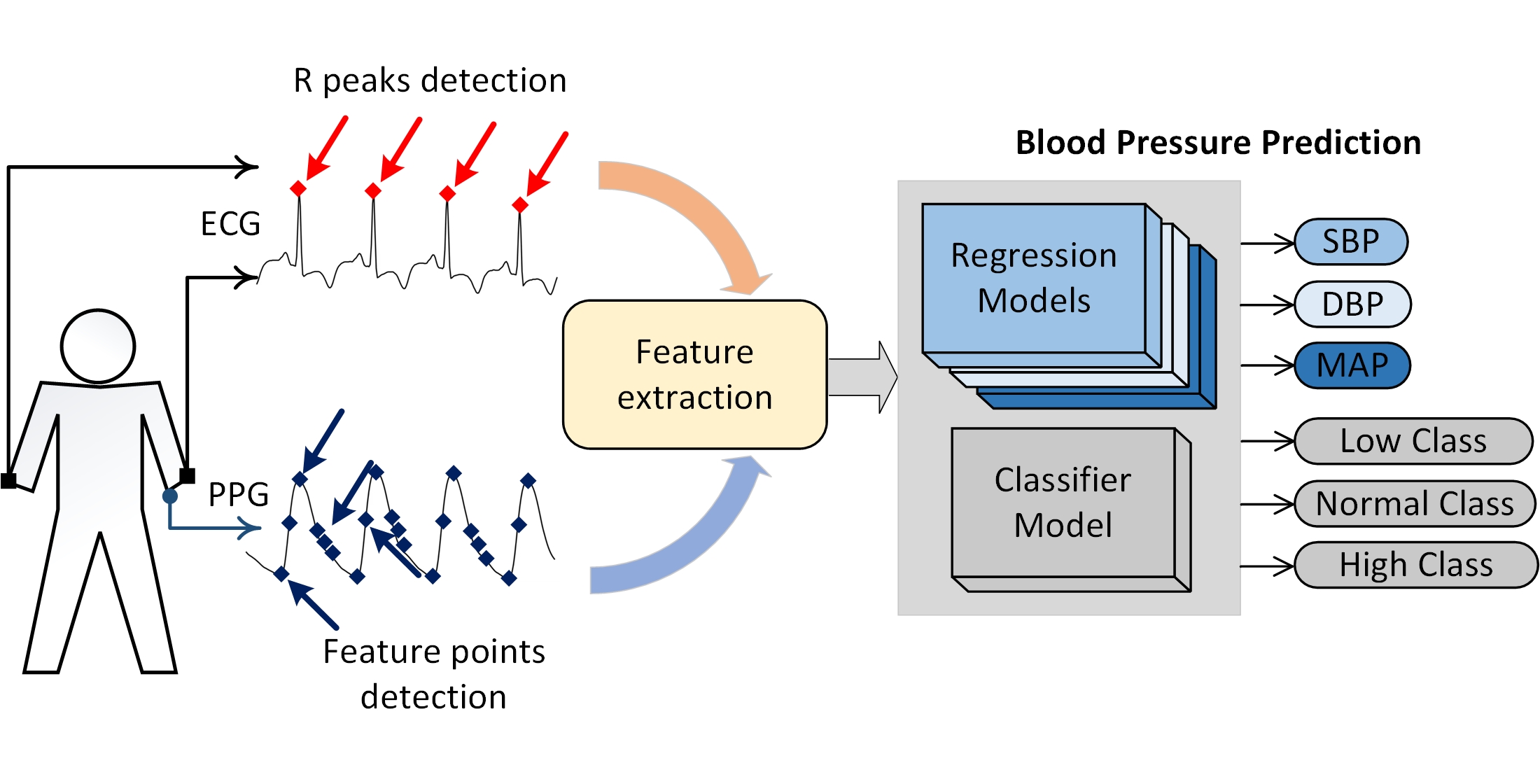
Determining the level of blood pressure (BP) in a non-invasive way and without a sphygmomanometer cuff is of great relevance when conducting continuous monitoring or screening studies. In this regard, a method for predicting BP parameters based on the signals of the photoplethysmogram (PPG) and electrocardiogram (ECG) signals has been developed. It is proposed to use, as informative features, the time of pulse wave propagation (PTT) and a set of calculated pulse parameters of PPG. PTT is defined as the time intervals between the R-wave of the ECG and the corresponding characteristic points on the PPG acquired optically from the finger. As parameters of the PPG pulse, the known characteristics of this signal described in the literature are used, as well as additional informative features selected during the study.
In accordance with the above, the tools of machine learning theory were used to construct a classifier model and regression models. The approach described in this paper to determine BP makes it possible to use 10-second ECG signals in any of the 12 common leads and PPG signals from any optical type of sensor.
The built model of the classifier detects three levels of BP: low, normal, and high, at the accuracy metric=0.8494. The regression models predict systolic, diastolic, and mean BP parameters in accordance with the requirements of the British Hypertension Society (BHS) standard by the magnitude of the absolute error.
The proposed method for assessing the level of BP involves real-time measurements and can be used in the design of measuring equipment for screening studies, as well as in continuous monitoring tasks within the framework of BHS requirements.
References
- Zhou, B., Carrillo-Larco, R. M., Danaei, G., Riley, L. M., Paciorek, C. J., Stevens, G. A. et. al. (2021). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet, 398 (10304), 957–980. doi: https://doi.org/10.1016/s0140-6736(21)01330-1
- Hypertension (2021). World Health Organization (WHO). Available at: https://www.who.int/en/news-room/fact-sheets/detail/hypertension
- Williams, B., Mancia, G., Spiering, W., Agabiti Rosei, E., Azizi, M., Burnier, M. et. al. (2018). 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal, 39 (33), 3021–3104. doi: https://doi.org/10.1093/eurheartj/ehy339
- Peter, L., Noury, N., Cerny, M. (2014). A review of methods for non-invasive and continuous blood pressure monitoring: Pulse transit time method is promising? IRBM, 35 (5), 271–282. doi: https://doi.org/10.1016/j.irbm.2014.07.002
- Pandit, J. A., Lores, E., Batlle, D. (2020). Cuffless Blood Pressure Monitoring. Clinical Journal of the American Society of Nephrology, 15 (10), 1531–1538. doi: https://doi.org/10.2215/cjn.03680320
- Mukkamala, R., Stergiou, G. S., Avolio, A. P. (2022). Cuffless Blood Pressure Measurement. Annual Review of Biomedical Engineering, 24 (1), 203–230. doi: https://doi.org/10.1146/annurev-bioeng-110220-014644
- Figini, V., Galici, S., Russo, D., Centonze, I., Visintin, M., Pagana, G. (2022). Improving Cuff-Less Continuous Blood Pressure Estimation with Linear Regression Analysis. Electronics, 11 (9), 1442. doi: https://doi.org/10.3390/electronics11091442
- Stergiou, G. S., Mukkamala, R., Avolio, A., Kyriakoulis, K. G., Mieke, S., Murray, A. et. al. (2022). Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. Journal of Hypertension, 40 (8), 1449–1460. doi: https://doi.org/10.1097/hjh.0000000000003224
- Nour, M., Polat, K. (2020). Automatic Classification of Hypertension Types Based on Personal Features by Machine Learning Algorithms. Mathematical Problems in Engineering, 2020, 1–13. doi: https://doi.org/10.1155/2020/2742781
- Ibrahim, B., Nathan, V., Jafari, R. (2017). Exploration and validation of alternate sensing methods for wearable continuous pulse transit time measurement using optical and bioimpedance modalities. 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). doi: https://doi.org/10.1109/embc.2017.8037256
- Thambiraj, G., Gandhi, U., Mangalanathan, U., Jose, V. J. M., Anand, M. (2020). Investigation on the effect of Womersley number, ECG and PPG features for cuff less blood pressure estimation using machine learning. Biomedical Signal Processing and Control, 60, 101942. doi: https://doi.org/10.1016/j.bspc.2020.101942
- Saeed, M., Villarroel, M., Reisner, A. T., Clifford, G., Lehman, L.-W., Moody, G. et. al. (2011). Multiparameter Intelligent Monitoring in Intensive Care II: A public-access intensive care unit database*. Critical Care Medicine, 39 (5), 952–960. doi: https://doi.org/10.1097/ccm.0b013e31820a92c6
- Sanuki, H., Fukui, R., Inajima, T., Warisawa, S. (2017). Cuff-less Calibration-free Blood Pressure Estimation under Ambulatory Environment using Pulse Wave Velocity and Photoplethysmogram Signals. Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies. doi: https://doi.org/10.5220/0006112500420048
- Liang, Y., Chen, Z., Ward, R., Elgendi, M. (2018). Hypertension Assessment via ECG and PPG Signals: An Evaluation Using MIMIC Database. Diagnostics, 8 (3), 65. doi: https://doi.org/10.3390/diagnostics8030065
- Miao, F., Liu, Z.-D., Liu, J.-K., Wen, B., He, Q.-Y., Li, Y. (2020). Multi-Sensor Fusion Approach for Cuff-Less Blood Pressure Measurement. IEEE Journal of Biomedical and Health Informatics, 24 (1), 79–91. doi: https://doi.org/10.1109/jbhi.2019.2901724
- Hasanzadeh, N., Ahmadi, M. M., Mohammadzade, H. (2020). Blood Pressure Estimation Using Photoplethysmogram Signal and Its Morphological Features. IEEE Sensors Journal, 20 (8), 4300–4310. doi: https://doi.org/10.1109/jsen.2019.2961411
- Kachuee, M., Kiani, M. M., Mohammadzade, H., Shabany, M. (2015). Cuff-less high-accuracy calibration-free blood pressure estimation using pulse transit time. 2015 IEEE International Symposium on Circuits and Systems (ISCAS). doi: https://doi.org/10.1109/iscas.2015.7168806
- DeMers, D., Wachs, D. (2022). Physiology, Mean Arterial Pressure. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK538226/
- Meng, L., Yu, W., Wang, T., Zhang, L., Heerdt, P. M., Gelb, A. W. (2018). Blood Pressure Targets in Perioperative Care. Hypertension, 72 (4), 806–817. doi: https://doi.org/10.1161/hypertensionaha.118.11688
- Guzman, J. C., Melin, P., Prado-Arechiga, G. (2017). Design of an Optimized Fuzzy Classifier for the Diagnosis of Blood Pressure with a New Computational Method for Expert Rule Optimization. Algorithms, 10 (3), 79. doi: https://doi.org/10.3390/a10030079
- Elgendi, M. (2012). On the Analysis of Fingertip Photoplethysmogram Signals. Current Cardiology Reviews, 8 (1), 14–25. doi: https://doi.org/10.2174/157340312801215782
- Scholkmann, F., Boss, J., Wolf, M. (2012). An Efficient Algorithm for Automatic Peak Detection in Noisy Periodic and Quasi-Periodic Signals. Algorithms, 5 (4), 588–603. doi: https://doi.org/10.3390/a5040588
- Kachuee, M., Kiani, M. M., Mohammadzade, H., Shabany, M. (2017). Cuffless Blood Pressure Estimation Algorithms for Continuous Health-Care Monitoring. IEEE Transactions on Biomedical Engineering, 64 (4), 859–869. doi: https://doi.org/10.1109/tbme.2016.2580904
- Hasan, O. S., Saleh, I. A. (2021). Development of heart attack prediction model based on ensemble learning. Eastern-European Journal of Enterprise Technologies, 4 (2 (112)), 26–34. doi: https://doi.org/10.15587/1729-4061.2021.238528
- Geurts, P., Ernst, D., Wehenkel, L. (2006). Extremely randomized trees. Machine Learning, 63 (1), 3–42. doi: https://doi.org/10.1007/s10994-006-6226-1
- Pedregosa, F. et. al. (2011). Scikit-learn: Machine Learning in Python. Journal of Machine Learning Research, 12, 2825–2830. Available at: https://www.jmlr.org/papers/volume12/pedregosa11a/pedregosa11a.pdf
- Chawla, N. V., Bowyer, K. W., Hall, L. O., Kegelmeyer, W. P. (2002). SMOTE: Synthetic Minority Over-sampling Technique. Journal of Artificial Intelligence Research, 16, 321–357. doi: https://doi.org/10.1613/jair.953
- Chen, T., Guestrin, C. (2016). XGBoost: A Scalable Tree Boosting System. Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. doi: https://doi.org/10.1145/2939672.2939785
- Wolpert, D. H. (1992). Stacked generalization. Neural Networks, 5 (2), 241–259. doi: https://doi.org/10.1016/s0893-6080(05)80023-1
- O'Brien, E., Petrie, J., Littler, W., de Swiet, M., Padfield, P. L., O'Malley, K. et. al. (1990). The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices with special reference to ambulatory systems. Journal of Hypertension, 8 (7), 607–619. doi: https://doi.org/10.1097/00004872-199007000-00004
- ANSI/AAMI SP10:2002/(R)2008 & ANSI/AAMI SP10:2002/A1:2003/(R)2008 & ANSI/AAMI SP10:2002/A2:2006/(R)2008. Manual, electronic, or automated sphygmomanometers. Association for the Advancement of Medical Instrumentation.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Alexey Savostin, Amandyk Tuleshov, Kayrat Koshekov, Galina Savostina, Alexandr Largin

This work is licensed under a Creative Commons Attribution 4.0 International License.
The consolidation and conditions for the transfer of copyright (identification of authorship) is carried out in the License Agreement. In particular, the authors reserve the right to the authorship of their manuscript and transfer the first publication of this work to the journal under the terms of the Creative Commons CC BY license. At the same time, they have the right to conclude on their own additional agreements concerning the non-exclusive distribution of the work in the form in which it was published by this journal, but provided that the link to the first publication of the article in this journal is preserved.
A license agreement is a document in which the author warrants that he/she owns all copyright for the work (manuscript, article, etc.).
The authors, signing the License Agreement with TECHNOLOGY CENTER PC, have all rights to the further use of their work, provided that they link to our edition in which the work was published.
According to the terms of the License Agreement, the Publisher TECHNOLOGY CENTER PC does not take away your copyrights and receives permission from the authors to use and dissemination of the publication through the world's scientific resources (own electronic resources, scientometric databases, repositories, libraries, etc.).
In the absence of a signed License Agreement or in the absence of this agreement of identifiers allowing to identify the identity of the author, the editors have no right to work with the manuscript.
It is important to remember that there is another type of agreement between authors and publishers – when copyright is transferred from the authors to the publisher. In this case, the authors lose ownership of their work and may not use it in any way.








