IoT system development for heart rhythm monitoring and cardiovascular risk estimation
DOI:
https://doi.org/10.15587/1729-4061.2024.299068Keywords:
cardiovascular risk, free hardware, heart rate variability, systems estimation, IoT systemAbstract
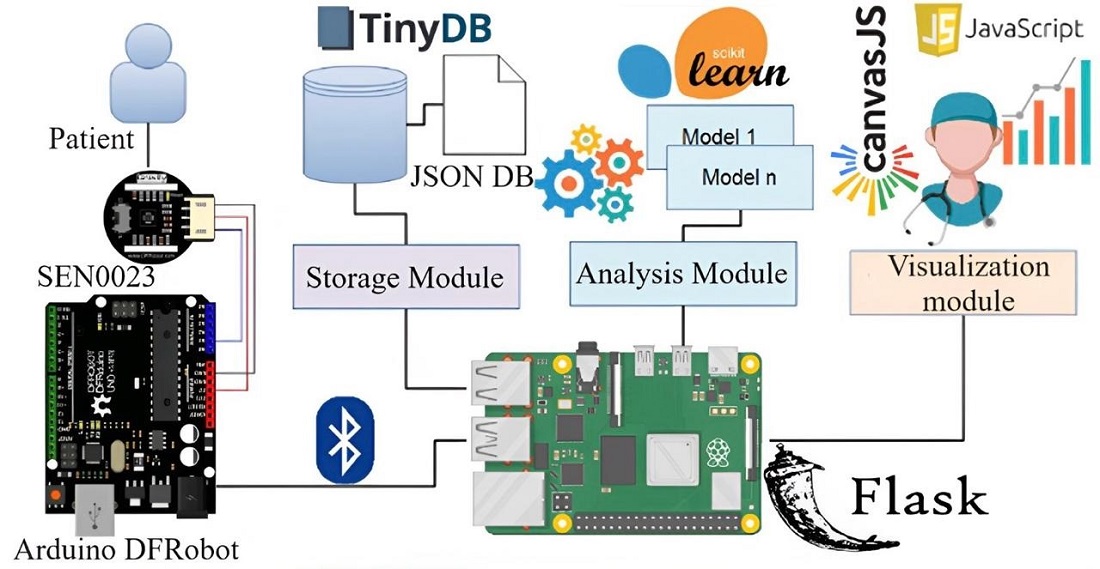
The research focuses on addressing the global issue of cardiovascular diseases. The key variable under consideration for predicting cardiovascular diseases is heart rate variability (HRV). Leveraging the widespread adoption of IoT in various applications, particularly in the health sector, the study proposes the design and implementation of an IoT system for HRV monitoring. The research unfolded in four methodological phases: exploration and selection of technologies, definition of the IoT architecture, development of the prototype, and verification of its functionality. The implemented IoT system adheres to the conventional 4-layer IoT architecture: capture, storage, analysis, and visualization. Heart rate data is periodically acquired using a heart rate sensor and an Arduino-compatible board. The storage layer employs a non-relational database to store the captured data. The analysis layer extracts metrics related to HRV (High: RR <750 ms, Moderate: RR 750–900 ms, Low: RR >900 ms) by applying and delivering quantitative results from clustering algorithms such as machine learning models to evaluate data distribution. Risk levels indicate specific patient metrics. Thus, a 75-year-old patient exhibits an average HR of 75.56, Avg. RR of 795.42, falling into Cluster 1 with a risk value of 1.0. Similar detailed metrics and risk stratifications are presented for patients aged 68, 46, 37, and 18, demonstrating the system's robustness and efficacy in assessing cardiovascular risk. The visualization layer enables real-time observation of physiological variables, risk metrics, and results from data analytics models. The distinctive features of the results lie in the portability advantages of the IoT system, utilizing free hardware and software tools. This facilitates easy replication and utilization of the proposed system in medical campaigns, specifically for the early detection of cardiac conditions. The portable IoT system, leveraging free tools, enhances predictive capabilities for early cardiovascular risk detection globally
Supporting Agency
- The authors would like to thank the Universidad de Cartagena-Colombia for their support in the development of this research.
References
- Zakutynskyi, I., Sibruk, L., Rabodzei, I. (2023). Performance evaluation of the cloud computing application for IoT-based public transport systems. Eastern-European Journal of Enterprise Technologies, 4 (9 (124)), 6–13. https://doi.org/10.15587/1729-4061.2023.285514
- Conti, M., Dehghantanha, A., Franke, K., Watson, S. (2018). Internet of Things security and forensics: Challenges and opportunities. Future Generation Computer Systems, 78, 544–546. https://doi.org/10.1016/j.future.2017.07.060
- Naveen, S., Hegde, S. (2016). Study of IoT: Understanding IoT Architecture, Applications, Issues and Challenges. International Journal of Advanced Networking & Applications (IJANA), 477–482. Available at: http://www.ijana.in/Special Issue/S105.pdf
- Dorsemaine, B., Gaulier, J.-P., Wary, J.-P., Kheir, N., Urien, P. (2015). Internet of Things: A Definition & Taxonomy. 2015 9th International Conference on Next Generation Mobile Applications, Services and Technologies. https://doi.org/10.1109/ngmast.2015.71
- Terokhin, V., Stervoyedov, M., Ridozub, O. (2021). Design and implementation of the distributed dosimetric system based on the principles of IoT. Eastern-European Journal of Enterprise Technologies, 5 (9 (113)), 91–100. https://doi.org/10.15587/1729-4061.2021.243153
- Rani, R., Kashyap, V., Khurana, M. (2022). Role of IoT-Cloud Ecosystem in Smart Cities : Review and Challenges. Materials Today: Proceedings, 49, 2994–2998. https://doi.org/10.1016/j.matpr.2020.10.054
- Atzori, L., Iera, A., Morabito, G. (2017). Understanding the Internet of Things: definition, potentials, and societal role of a fast evolving paradigm. Ad Hoc Networks, 56, 122–140. https://doi.org/10.1016/j.adhoc.2016.12.004
- Chatterjee, S., Kar, A. K., Gupta, M. P. (2018). Success of IoT in Smart Cities of India: An empirical analysis. Government Information Quarterly, 35 (3), 349–361. https://doi.org/10.1016/j.giq.2018.05.002
- Zhang, C. (2020). Design and application of fog computing and Internet of Things service platform for smart city. Future Generation Computer Systems, 112, 630–640. https://doi.org/10.1016/j.future.2020.06.016
- Zakutynskyi, I., Rabodzei, I., Burmakin, S., Kalishuk, O., Nebylytsia, V. (2023). Improving a procedure of load balancing in distributed IoT systems. Eastern-European Journal of Enterprise Technologies, 5 (2 (125)), 6–22. https://doi.org/10.15587/1729-4061.2023.287790
- Konyrova, M., Kumyzbayeva, S., Iliev, T., Chezhimbayeva, K. (2023). Effeciency assessment of IoT devices control with Teletraffic theory. Eastern-European Journal of Enterprise Technologies, 3 (9 (123)), 49–59. https://doi.org/10.15587/1729-4061.2023.281287
- Viloria Núñez, C. A., Sanmartín Mendoza, P., Avila Hernández, K., Jabba Molinares, D. (2022). Internet de las cosas y la salud centrada en el hogar. Salud Uninorte, 32 (02), 337–351. https://doi.org/10.14482/sun.32.2.8954
- Liu, Y., Niu, J., Yang, L., Shu, L. (2014). eBPlatform: An IoT-based system for NCD patients homecare in China. 2014 IEEE Global Communications Conference. https://doi.org/10.1109/glocom.2014.7037175
- Alsaydia, O. M., Saadallah, N. R., Malallah, F. L., AL-Adwany, M. A. S. (2021). Limiting COVID-19 infection by automatic remote face mask monitoring and detection using deep learning with IoT. Eastern-European Journal of Enterprise Technologies, 5 (2 (113)), 29–36. https://doi.org/10.15587/1729-4061.2021.238359
- Veloza, L., Jiménez, C., Quiñones, D., Polanía, F., Pachón-Valero, L. C., Rodríguez-Triviño, C. Y. (2019). Variabilidad de la frecuencia cardiaca como factor predictor de las enfermedades cardiovasculares. Revista Colombiana de Cardiología, 26 (4), 205–210. https://doi.org/10.1016/j.rccar.2019.01.006
- Pardo-Fresno, M., Fernández-Barbeira, S., González-Bermúdez, I. (2011). Assessment and management of Bradycardias in Primary Care emergencies. Primary Care Notebooks, 8, 107–110.
- Osanai, H. (2011). Hear rate variability during a 24-hour period recorded with a Polar heart rate monitor. Autonomic Neuroscience, 165 (2), 210. https://doi.org/10.1016/j.autneu.2011.08.013
- Wang, L., Lin, Y., Wang, J. (2019). A RR interval based automated apnea detection approach using residual network. Computer Methods and Programs in Biomedicine, 176, 93–104. https://doi.org/10.1016/j.cmpb.2019.05.002
- Kiran kumar, C., Manaswini, M., Maruthy, K. N., Siva Kumar, A. V., Mahesh kumar, K. (2021). Association of Heart rate variability measured by RR interval from ECG and pulse to pulse interval from Photoplethysmography. Clinical Epidemiology and Global Health, 10, 100698. https://doi.org/10.1016/j.cegh.2021.100698
- Islam, M. N., Raiyan, K. R., Mitra, S., Mannan, M. M. R., Tasnim, T., Putul, A. O., Mandol, A. B. (2023). Predictis: an IoT and machine learning-based system to predict risk level of cardio-vascular diseases. BMC Health Services Research, 23 (1). https://doi.org/10.1186/s12913-023-09104-4
- Hudhajanto, R. P., Mulyadi, I. H., Sandi, A. A. (2022). Wearable Sensor Device berbentuk Face Shield untuk Memonitor Detak Jantung berbasis IoT. Journal of Applied Informatics and Computing, 6 (1), 87–92. https://doi.org/10.30871/jaic.v6i1.4105
- Goumopoulos, C., Menti, E. (2019). Stress Detection in Seniors Using Biosensors and Psychometric Tests. Procedia Computer Science, 152, 18–27. https://doi.org/10.1016/j.procs.2019.05.022
- de la Cruz Torres, B., Lopez, C. L., Orellana, J. N. (2008). Analysis of heart rate variability at rest and during aerobic exercise: a study in healthy people and cardiac patients. British Journal of Sports Medicine, 42 (9), 715–720. https://doi.org/10.1136/bjsm.2007.043646
- Delgado, D., Girón, D., Chanchí, G., Márceles, K., Dionizio, S. (2019). System for the Detection and Monitoring of Heart Disease Supported in SBC. Iberian Journal of Information Systems and Technologies, 717–728. Available at: http://risti.xyz/issues/ristie17.pdf
- Pérez, A., Guerra, J. L. (2014). Implementation of a heart rate query and measurement module with GSM data sending using Open Hardware. In: XXI International Congress of Electronic, Electrical and Computer Engineering - INTERCON 2014. Arequipa - Perú.
- Chanchi, G. E., Ospina, M. A., Pérez, J. L. (2020). IoT system to monitoring heart rate variability in usability tests. Journal Spaces, 41 (25), 84–97. Available at: https://www.revistaespacios.com/a20v41n25/20412507.html
- Cano-Contreras, M., Andrade-Ceballos, G., Vargas-Cano, P., Villanueva-Pérez, N. (2017). Low cost Arduino based heart rate monitor. Journal of Technologies in Industrial Processes, 1 (1), 21–25. Available at: https://www.ecorfan.org/taiwan/research_journals/Tecnologias_en_Procesos_Industriales/vol1num1/Revista_de_Tecnolog%C3%ADas_en_Procesos_Industriales_V1_N1_3.pdf
- Piedrahita-Gonzalez, J., Cubillos-Calvachi, J., Gutiérrez-Ardila, C., Montenegro-Marin, C., Gaona-García, P. (2018). IOT System for Self-diagnosis of Heart Diseases Using Mathematical Evaluation of Cardiac Dynamics Based on Probability Theory. Smart Innovation, Systems and Technologies, 433–441. https://doi.org/10.1007/978-3-030-03577-8_48
- Santos, M. A. G., Munoz, R., Olivares, R., Filho, P. P. R., Ser, J. D., Albuquerque, V. H. C. de. (2020). Online heart monitoring systems on the internet of health things environments: A survey, a reference model and an outlook. Information Fusion, 53, 222–239. https://doi.org/10.1016/j.inffus.2019.06.004
- Anuhya Ardeti, V., Ratnam Kolluru, V., Routray, S., Omkar Lakshmi Jagan, B., Kishore Kumar, A., Ramachandran, R. et al. (2024). Development of real time ECG monitoring and unsupervised learning classification framework for cardiovascular diagnosis. Biomedical Signal Processing and Control, 88, 105553. https://doi.org/10.1016/j.bspc.2023.105553
- Rahman, M. Z., Akbar, M. A., Leiva, V., Tahir, A., Riaz, M. T., Martin-Barreiro, C. (2023). An intelligent health monitoring and diagnosis system based on the internet of things and fuzzy logic for cardiac arrhythmia COVID-19 patients. Computers in Biology and Medicine, 154, 106583. https://doi.org/10.1016/j.compbiomed.2023.106583
- Montoya, E. A. Q., Colorado, S. F. J., Muñoz, W. Y. C., Golondrino, G. E. C. (2017). Propuesta de una Arquitectura para Agricultura de Precisión Soportada en IoT. RISTI - Revista Ibérica de Sistemas e Tecnologias de Informação, 24, 39–56. https://doi.org/10.17013/risti.24.39-56
- Webster, J. G. (Ed.) (2014). The Physiological Measurement Handbook. CRC Press. https://doi.org/10.1201/b17831
- Young, D. W. (2014). Self-measure of heart rate variability (HRV) and arrhythmia to monitor and to manage atrial arrhythmias: personal experience with high intensity interval exercise (HIIE) for the conversion to sinus rhythm. Frontiers in Physiology, 5. https://doi.org/10.3389/fphys.2014.00251
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Martín Emilo Monroy, Gabriel Elías Chanchí, Manuel Alejandro Ospina

This work is licensed under a Creative Commons Attribution 4.0 International License.
The consolidation and conditions for the transfer of copyright (identification of authorship) is carried out in the License Agreement. In particular, the authors reserve the right to the authorship of their manuscript and transfer the first publication of this work to the journal under the terms of the Creative Commons CC BY license. At the same time, they have the right to conclude on their own additional agreements concerning the non-exclusive distribution of the work in the form in which it was published by this journal, but provided that the link to the first publication of the article in this journal is preserved.
A license agreement is a document in which the author warrants that he/she owns all copyright for the work (manuscript, article, etc.).
The authors, signing the License Agreement with TECHNOLOGY CENTER PC, have all rights to the further use of their work, provided that they link to our edition in which the work was published.
According to the terms of the License Agreement, the Publisher TECHNOLOGY CENTER PC does not take away your copyrights and receives permission from the authors to use and dissemination of the publication through the world's scientific resources (own electronic resources, scientometric databases, repositories, libraries, etc.).
In the absence of a signed License Agreement or in the absence of this agreement of identifiers allowing to identify the identity of the author, the editors have no right to work with the manuscript.
It is important to remember that there is another type of agreement between authors and publishers – when copyright is transferred from the authors to the publisher. In this case, the authors lose ownership of their work and may not use it in any way.









